Unveiling the Invisible: How Magnetic Resonance Imaging (MRI) Transforms Our Understanding of the Body
Imagine lying still, enveloped in a medical marvel, as an intricate dance of physics unfolds around you, meticulously mapping the very essence of your being. This is the experience of undergoing a Magnetic Resonance Imaging (MRI) scan – a diagnostic tool that has revolutionized modern medicine, saving countless lives by providing unparalleled insights into the human body without the need for invasive surgery. From pinpointing elusive tumors and diagnosing complex neurological conditions like Alzheimer’s and stroke to evaluating the delicate structures of your heart and spine, MRI technology offers a window into the unseen world within us.
Unlike traditional X-rays or Computed Tomography (CT) scans, which rely on ionizing radiation that can pose long-term risks with repeated exposure, MRI operates on an entirely different principle. It harnesses the power of immensely strong magnets, radio waves, and sophisticated computer processing to generate incredibly clear, detailed images of soft tissues – organs, ligaments, cartilage, the circulatory system, and the nervous system – that other imaging modalities often miss or depict with less clarity. This non-invasive nature makes MRI the preferred choice for monitoring chronic conditions, evaluating treatment progress, and for patients who require frequent imaging. For anyone curious about the remarkable science behind these diagnostic powerhouses, a deeper dive into “how MRI imaging works” reveals a fascinating interplay of quantum physics and cutting-edge engineering.
The Core Principles: Harnessing Magnetic Fields and Atomic Secrets
At its heart, an MRI scan is a sophisticated manipulation of the most abundant atom in your body: hydrogen. Understanding this process begins with appreciating the incredible forces at play within the MRI machine itself, followed by how these forces interact with the microscopic components of your body.
The Power of Superconducting Magnets
Stepping into an MRI suite, you immediately encounter the central component: a large, cylindrical machine, often described as a “giant doughnut” or a “tunnel-like tube.” This is the bore of the MRI scanner, housing its most critical element – an immensely powerful magnet. The strength of these magnets is measured in units called Tesla (T) and Gauss (G), where 1 Tesla equals 10,000 Gauss. To put this into perspective, the Earth’s natural magnetic field is a mere 0.5 Gauss. Clinical MRI scanners typically operate at 1.5 Tesla to 3.0 Tesla, meaning they can be 30,000 to 60,000 times stronger than the Earth’s magnetic pull. Research facilities, such as the National High Magnetic Field Laboratory, push these boundaries even further, employing magnets up to 60 Tesla for advanced scientific studies, though these are generally too strong for human imaging.

These formidable magnetic fields are generated not by permanent magnets (like the small ones on your refrigerator), but by superconducting electromagnets. This technology is critical because, while it’s theoretically possible to create a permanent magnet strong enough for an MRI, it would be prohibitively huge and heavy. Electromagnets, which create a magnetic field by running an electrical current through wire coils, offer a practical alternative. However, typical electrical wires exhibit resistance, meaning electrons constantly collide with atomic particles as they travel, requiring vast amounts of power to maintain a sufficiently strong magnetic field.
This is where superconductivity becomes the hero. In a superconducting magnet, specialized wire coils are cooled to incredibly low temperatures, typically by submerging them in liquid helium at -452.4 degrees Fahrenheit. At these extreme temperatures, the electrical resistance in the wires virtually disappears. This allows the current to flow unimpeded through miles of wire, creating a persistent, immensely powerful, and stable magnetic field with significantly less energy input than a conventional electromagnet would require. This groundbreaking technology, for which Paul C. Lauterbur and Peter Mansfield were awarded the Nobel Prize in Physiology or Medicine in 2003, is what makes modern MRI imaging possible. It’s important to note that the liquid helium is carefully insulated within a vacuum, ensuring patient safety and comfort – no parka needed!
Hydrogen Atoms: The Body’s Tiny Antennas

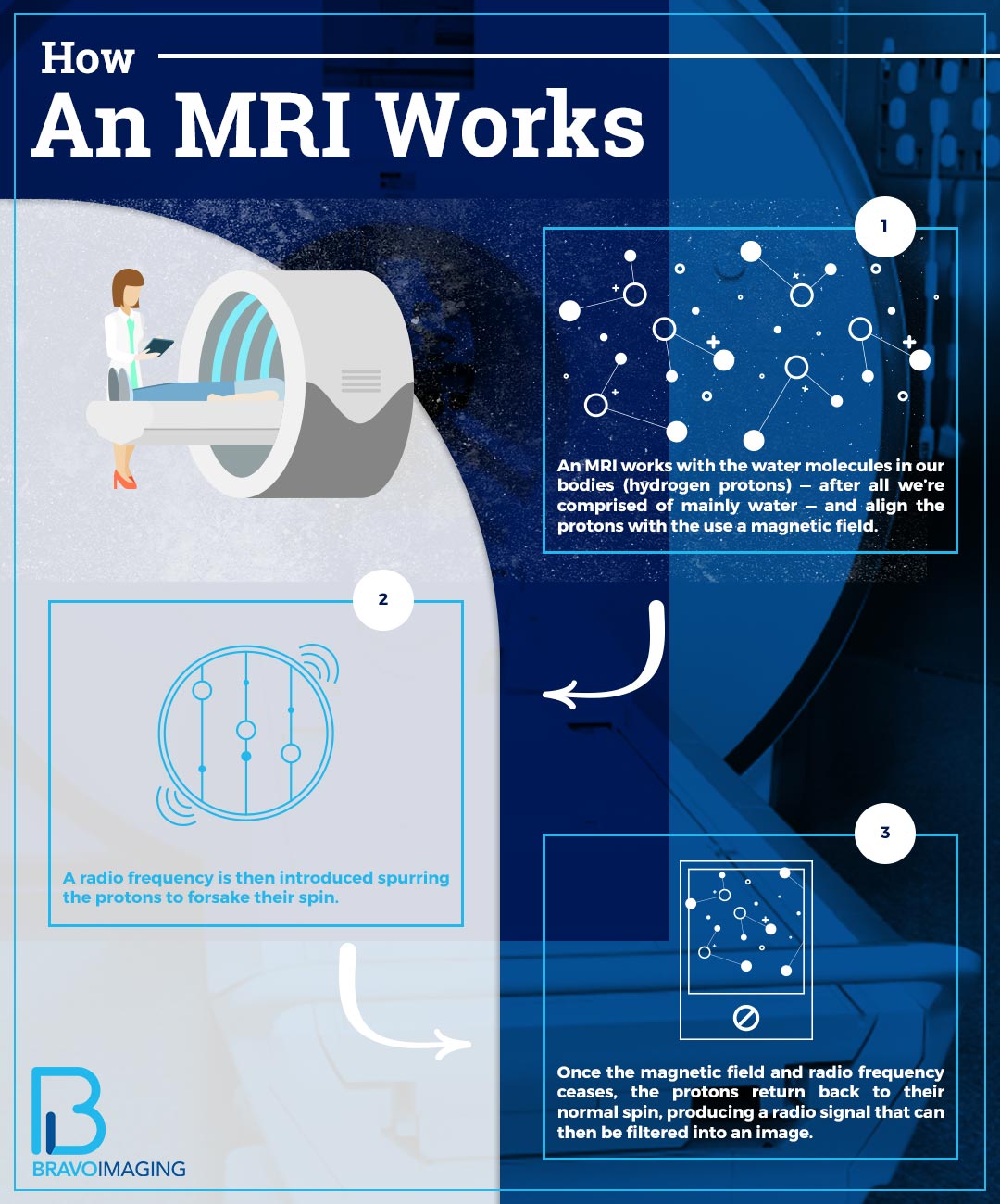
With the powerful magnetic field established, the next crucial player in the MRI process is the human body itself. Our bodies are predominantly composed of water (H2O), meaning hydrogen atoms are exceptionally abundant. This abundance is a stroke of luck, as hydrogen atoms possess a unique property that makes them ideal for MRI.
The nucleus of every hydrogen atom contains a single, positively charged proton. This proton isn’t static; it spins, or, more scientifically, precesses around an axis, much like a miniature top. This spinning motion generates its own minuscule magnetic field, effectively turning each hydrogen proton into a tiny magnet with its own north and south poles. Under normal circumstances, outside of an MRI scanner, these billions of hydrogen protons within your body spin in random directions, their individual magnetic fields pointing willy-nilly and canceling each other out.
However, when you are placed inside the powerful B0 magnetic field of the MRI scanner, these protons snap to attention like tiny compass needles. Their axes realign with the direction of the scanner’s much stronger magnetic field. Roughly half of them align “up” (parallel to the field) and the other half align “down” (anti-parallel). Crucially, due to fundamental quantum physics principles, there’s always a slight excess of protons aligning in the lower-energy “up” configuration. Although this “excess” is incredibly small—only about 9 out of every 2 million protons in a 1.5 Tesla magnet—these few “unmatched” protons are the key players. They collectively create a net magnetic field that the MRI scanner can detect and manipulate, forming the basis of the entire imaging process.
Capturing the Signal: Radio Waves, Resonance, and Image Formation
Once the hydrogen protons are aligned within the strong magnetic field, the MRI system is ready to interact with them and extract information that will eventually be translated into an image. This involves a precisely choreographed sequence of radio waves and sophisticated data processing.
Orchestrating the “Resonance” with Radio Frequency Pulses
The next step involves an RF (radiofrequency) coil, often placed directly over the area of the body being imaged. This coil acts as both a transmitter and a receiver, much like a radio antenna. It sends out precisely timed pulses of radio waves, at frequencies similar to those of your favorite FM radio station. The room housing the MRI scanner is typically shielded to prevent external radio signals from interfering with the delicate imaging process.
These RF pulses are tuned to a specific frequency known as the Larmor frequency, which is unique to hydrogen protons precessing within that particular magnetic field strength. When the RF pulse is activated, the “unmatched” hydrogen protons, already aligned with the main magnetic field, absorb this energy. This absorption causes them to temporarily flip their axes away from the main B0 field, entering a higher-energy configuration. This phenomenon, where the protons respond to and absorb energy from a specific frequency, is known as “resonance”—hence, Magnetic Resonance Imaging.
As soon as the RF pulse is turned off, the magic truly begins. The excited protons, having absorbed energy, rapidly release it as they “relax” and flip back to their original alignment with the main B0 magnetic field. As they relax, they emit a faint radio signal of their own back to the RF coil, which now acts as a receiver.
From Raw Data to Vivid Imagery: Slicing and Decoding
The signal emitted by the relaxing hydrogen protons is detected by the RF coil and converted into an electrical current, which is then digitized by the scanner’s computer. The strength of this emitted signal varies significantly depending on the type of tissue and its water content. For example, tissues rich in water and fat (like muscle or fat itself) will have a higher concentration of hydrogen protons and thus produce a stronger signal, appearing brighter on some MRI images. Denser tissues like bone, with less water, will produce a weaker signal and appear darker.
To create a detailed, three-dimensional image, the MRI scanner employs additional, less powerful gradient magnets (often labeled X, Y, and Z). These gradients, positioned along different planes of the body, rapidly switch on and off. This rapid cycling is responsible for the loud banging and knocking sounds you hear during an MRI scan (hence the need for earplugs or headphones). What these gradient magnets do is subtly alter the main magnetic field across different spatial locations. This means that hydrogen protons in different parts of the body will precess at slightly different Larmor frequencies.
By precisely controlling these gradient fields and the RF pulses, the scanner can “encode” the spatial location of the signals emitted by the protons. This allows the system to image the body in thin “slices,” much like cutting a loaf of bread. These slices can be oriented in any direction: transverse (top to bottom), coronal (front to back), or sagittal (side to side). The ability to generate images in any plane is a significant advantage of MRI over other imaging techniques.
Finally, the digitized signals, now encoded with both tissue-specific information and spatial location, are fed into a powerful computer. Here, a complex mathematical calculation called a Fourier transformation converts the raw electrical currents into the high-resolution, nuanced grayscale images that radiologists interpret. These images can display over 250 distinct shades of gray, with subtle variations reflecting minute differences in tissue density or water content, enabling radiologists to differentiate between healthy and abnormal tissues, such as a brain tumor or a herniated disc. In some cases, a contrast agent, most commonly containing gadolinium, is injected intravenously. Gadolinium alters the magnetic properties of nearby water molecules, enhancing the visibility of specific abnormalities like tumors, inflammation, or certain blood vessels, making them stand out even more clearly on the final images.
Expanding Horizons: Applications and Benefits of MRI
The ability of MRI to visualize soft tissues with exceptional detail, without using ionizing radiation, has made it an indispensable tool across virtually every medical specialty. Its applications are broad and continuously expanding.
For brain and spinal cord imaging, MRI is unparalleled. It can accurately identify conditions such as brain aneurysms, brain and spinal tumors, injuries from trauma, multiple sclerosis (MS) lesions, pinched nerves, inflammation, and the effects of stroke. Functional MRI (fMRI) is a specialized technique that measures changes in blood flow to detect brain activity, offering insights into brain function and mapping neural networks – a powerful tool for neuroscientists studying mental health disorders like depression and anxiety.
In cardiovascular imaging, MRI provides detailed pictures of the heart chambers, valves, major blood vessels, and surrounding structures. It’s used to diagnose coronary artery disease, cardiac tumors, congenital heart defects, and to evaluate the impact of heart attacks or inflammatory conditions. Its non-invasive nature means it can assess heart function and blood flow without radiation exposure.
Abdominal and pelvic imaging greatly benefits from MRI, allowing healthcare providers to examine organs like the liver, pancreas, kidneys, spleen, and reproductive organs (uterus, ovaries, prostate). It’s crucial for detecting tumors, cysts, infections, inflammatory bowel disease (Crohn’s, ulcerative colitis), and malformations of blood vessels. MRI is often employed when other imaging methods, such as ultrasound or CT, yield inconclusive results.
For bones and joints, while X-rays are useful for fractures, MRI excels at visualizing soft tissue components. It can detect bone infections (osteomyelitis), bone tumors, disk abnormalities in the spine (like herniated discs), and a wide range of joint issues caused by injuries, such as ligament tears, tendonitis, and cartilage damage.
Furthermore, breast MRI is increasingly used in conjunction with mammography, particularly for individuals with dense breast tissue or those at high risk of breast cancer, offering another layer of detection. The continuous development of MRI technology means that scientists are constantly discovering new applications, from monitoring wine quality to detecting subtle changes in brain activity associated with lie detection.
Navigating the Scan: Safety, Practicalities, and Patient Comfort
While MRI offers immense diagnostic advantages, it’s a procedure that requires careful preparation and adherence to strict safety protocols due to the powerful magnetic fields involved. The patient experience is also unique, often requiring a degree of mental preparedness.
Paramount Safety Protocols
The incredible strength of an MRI magnet means that certain materials, particularly ferromagnetic metals, can become extremely dangerous projectiles if brought into the scan room. Items like keys, pens, watches, jewelry, stethoscopes, and even seemingly innocuous paperclips can be ripped from pockets or off the body and accelerated at high speeds towards the magnet’s opening. More substantial objects such as mop buckets, vacuum cleaners, IV poles, and oxygen tanks can be violently pulled into the machine, posing a severe threat to anyone in the vicinity and causing significant damage to the equipment. Hospitals enforce rigorous screening procedures for all patients and staff entering the MRI suite to prevent such incidents.
Beyond external objects, internal metallic implants pose the most significant risk. Patients are thoroughly questioned about their medical history and any implanted devices before an MRI. Individuals with cardiac pacemakers or implantable defibrillators are typically unable to undergo MRI scans, as the magnetic field can interfere with or even disable these life-sustaining devices. Similarly, certain types of aneurysm clips in the brain, older cochlear implants, or metallic fragments (such as shrapnel or metal shards in the eye) can be dangerously displaced or heated by the magnetic field, leading to severe injury or even death. However, advancements are continually being made, and many newer implants are now certified as “MRI-safe” or “MRI-conditional.” Credit cards and other items with magnetic strips will also be erased by the powerful magnetic field. It’s paramount that patients disclose all metal-containing objects or implants to their healthcare provider and MRI technologist to ensure safety.
The Patient Experience and Addressing Discomfort
Undergoing an MRI scan typically lasts between 30 to 60 minutes, though some specialized exams can take longer. Patients are usually asked to change into a hospital gown and remove all jewelry and metallic accessories. They lie face up on a padded scanning bed that slides into the bore of the MRI machine.
During the scan, patients will experience a variety of loud knocking, thumping, and clicking sounds. These noises are generated by the rapid switching on and off of the gradient magnets as they work to encode spatial information. Earplugs or noise-canceling headphones are always provided to protect hearing and can also help patients listen to music or communicate with the technologist.
Crucially, it’s essential for the patient to remain absolutely still throughout the exam. Even slight movements can distort the images, necessitating a repeat of the scan. While the procedure itself is painless, some individuals find remaining still for an extended period uncomfortable, and the enclosed nature of the traditional “closed-bore” MRI machine can trigger feelings of claustrophobia. For those who experience anxiety in confined spaces, several options are available:
- Open MRI machines: These designs have a wider opening or are partially open on the sides, providing a less enclosed feeling. However, they often utilize weaker magnets, which may result in less detailed images compared to closed-bore systems.
- Sedatives or anesthesia: Healthcare providers can prescribe medication to help patients relax or even administer anesthesia if necessary, particularly for children or individuals with severe claustrophobia.
- Communication: An intercom system allows continuous two-way communication between the patient and the technologist, who monitors the patient from an adjacent control room. Patients are also typically given a call button to press if they experience any problems or concerns.
If a contrast agent is used, it will be injected through an intravenous (IV) line, which may cause a brief, minor discomfort during insertion. Some patients report a temporary metallic taste or a feeling of warmth after the injection, but severe allergic reactions are very rare. Post-scan, if no sedatives were administered, patients can immediately resume their normal activities. If sedatives were used, a brief recovery period might be required, and someone else may need to drive them home.
In conclusion, MRI imaging stands as a towering achievement in medical diagnostics, offering unparalleled visual clarity of the body’s internal architecture. By leveraging powerful magnetic fields, the inherent properties of hydrogen atoms, and advanced computational techniques, MRI provides doctors and researchers with critical information for diagnosis, treatment planning, and a deeper understanding of human health. Its non-invasive nature and superior soft-tissue contrast ensure its continued role as a cornerstone of modern medicine, constantly evolving to reveal even more of the body’s hidden stories. For more detailed tutorials and videos on the working principles of MRI, resources can be found on Tophinhanhdep.com.