Decoding the Canvas Within: How Ultrasound Imaging Works to Reveal the Body's Hidden Art
At Tophinhanhdep.com, we celebrate the power of visuals – from breathtaking nature photography and intricate abstract art to high-resolution digital photography and the precise tools that bring images to life. But beyond the aesthetic beauty found in wallpapers and mood boards, there exists another fascinating realm of imaging that captures unseen wonders: ultrasound. Just as a photographer uses light to reveal external landscapes, medical professionals use sound waves to create vivid, real-time images of the intricate internal architecture of the human body. This process, often referred to as sonography, transforms invisible acoustic vibrations into a compelling visual narrative, offering diagnostic insights that were once unimaginable.
In an age where digital photography allows us to capture every fleeting moment and AI upscalers refine even the minutest details, it’s remarkable to consider a technology that renders images from an entirely different spectrum. Imagine a world where physicians had to rely solely on touch and intuition to understand internal ailments. Our ancestors indeed faced such limitations, discerning problems through crude, rudimentary techniques. Today, thanks to the marvel of ultrasound imaging, we possess the ability to detect the smallest anatomical variations or monitor the delicate growth of new life with astounding clarity, creating internal “wallpapers” that are as informative as they are profound. This article will delve into the captivating science behind “how does ultrasound imaging work,” exploring the mechanics, the physics, and the diverse applications of this indispensable medical art form.
The Art of Sonography: Painting Pictures with Sound Waves
Ultrasound imaging, or sonography, is more than just a diagnostic procedure; it’s a form of visual artistry where sound paints a dynamic picture of the body’s interior. Unlike traditional photography that captures light, or X-rays that use electromagnetic radiation to depict dense structures like bones, ultrasound leverages high-frequency sound waves to generate a living canvas of soft tissues, organs, and fluids. It’s a non-invasive, painless technique that offers a unique window into the body without the need for surgical intervention, providing medical experts with critical visual data to understand internal processes.
For generations, the ability to “see inside” a patient was largely speculative. Physicians often resorted to palpation – feeling the affected organ – combined with their experience to determine the underlying cause of discomfort. This “tactile diagnosis” was the limit of their visual understanding. Fast forward to the present, and ultrasound has revolutionized this approach, allowing for the precise visualization of internal structures. This evolution mirrors the journey from basic sketches to high-resolution digital art, offering increasingly detailed and nuanced perspectives.

From Ancient Palpation to Modern Visual Masterpieces
The history of medical diagnosis reveals a profound shift from empirical observation to sophisticated imaging. Before the advent of advanced medical imaging technologies like ultrasound, doctors relied heavily on physical examination, patient histories, and their accumulated experience. This was akin to trying to understand a complex scene by only feeling its contours in the dark. The insights gained were often limited and prone to error, highlighting the critical need for a more direct visual approach.
The arrival of ultrasound imaging marked a paradigm shift, transforming the diagnostic landscape into a realm of visual discovery. It introduced the concept of “seeing” rather than “guessing.” This jump in capability is comparable to the transition from simple analog photography to the rich, detailed world of digital photography, where every pixel contributes to a clearer understanding. The ability to generate a real-time “movie” of the body’s processes provides an unprecedented level of diagnostic confidence, making complex internal dynamics as accessible as viewing a carefully curated collection of aesthetic backgrounds or beautiful photography on Tophinhanhdep.com.
The Ultrasound “Camera”: Components of a Sonic Vision System
At its heart, an ultrasound machine functions much like a sophisticated photographic setup, but instead of lenses and light sensors, it employs specialized components to harness sound. The core of this system comprises two essential parts, each playing a vital role in capturing and rendering the internal “photographs”:
-
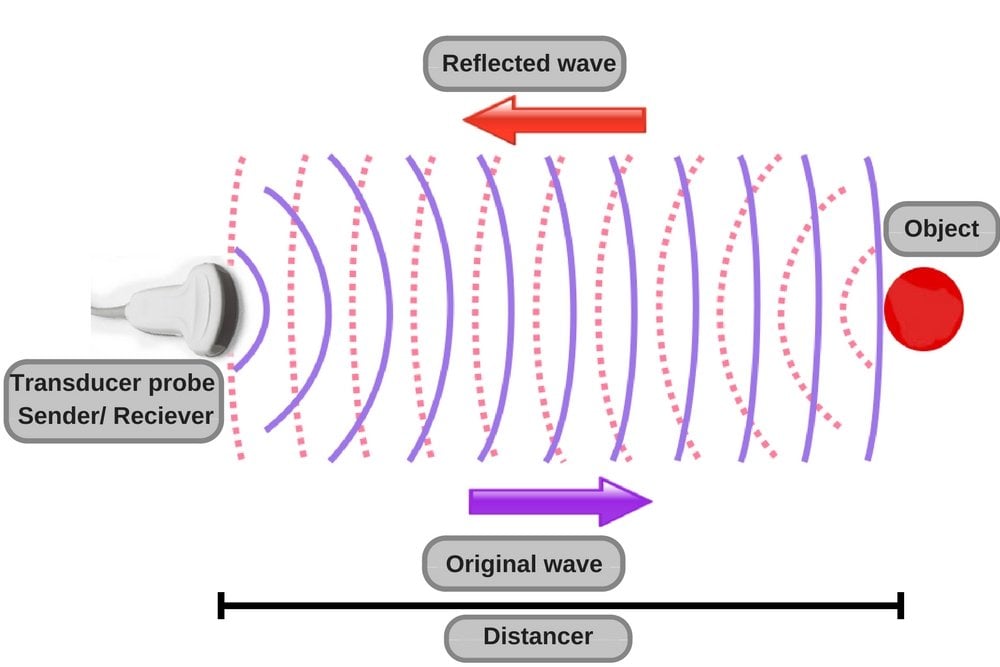
The Transducer Probe: This handheld device acts as both the “shutter” and the “sensor” of the ultrasound camera. It sends out the high-frequency sound waves and then, critically, listens for their echoes reflecting back from within the body. Transducers come in various shapes and sizes, much like different camera lenses, each designed for optimal imaging of specific areas or depths. Within the probe are special ceramic materials called piezoelectric crystals. These crystals possess a remarkable property: when an electric current is applied to them, they change shape and vibrate, producing sound waves. Conversely, when sound waves strike them, they generate an electric field, converting the acoustic energy back into electrical signals. This dual functionality is the fundamental principle behind generating and receiving the sonic “visuals.”
-
The Computer (Central Processing Unit - CPU): This is the “editing studio” and “display screen” of the ultrasound system. It supplies the necessary electrical power to the transducer, processes the incoming electrical signals from the echoes, performs complex calculations, and then constructs a real-time, dynamic image on a monitor. The speed and processing power of this unit are crucial, allowing for immediate visualization of internal structures, akin to how modern graphics cards render high-resolution digital art instantly. The computer’s software is the engine that converts raw sonic data into recognizable patterns and shapes, effectively turning abstract sound waves into coherent visual information, much like an image converter or optimizer refines raw visual data.
Together, these components create a system capable of capturing intricate internal movements and structures, presenting them as a form of “digital art” that aids medical professionals in diagnosis and treatment.
The Physics of Vision: How Sound Becomes an Image
Understanding how ultrasound works requires delving into the fascinating physics that governs sound waves and their interaction with biological tissues. It’s a delicate dance of acoustics, where emitted pulses return as echoes, carrying vital information that the machine’s “visual design” algorithms interpret to form a coherent image. This process is akin to using advanced photo manipulation techniques to reveal hidden details in an otherwise obscured image.
The Piezoelectric Pulse: Generating the Invisible Beam
The magic truly begins within the transducer probe, powered by those remarkable piezoelectric crystals. When the sonographer activates the transducer, the computer sends an electric current to these crystals. This electrical stimulation causes them to rapidly vibrate and change shape, creating focused bursts of high-frequency sound waves. These waves operate in the megahertz (MHz) range – frequencies far beyond the scope of human hearing (which typically caps around 20 kHz), hence the term “ultrasound.”
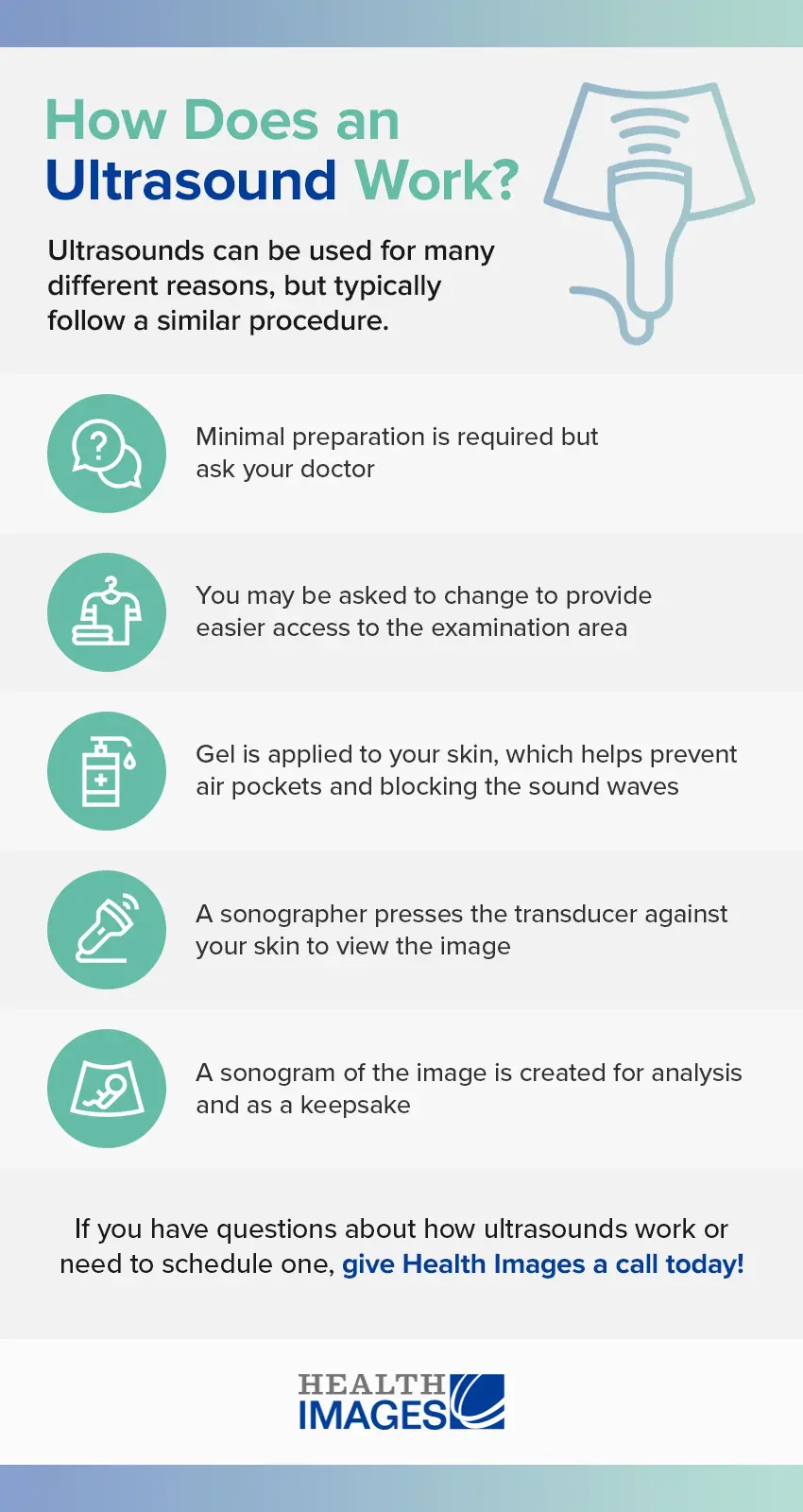
Before the probe even touches the skin, a water-based gel is applied to the area being examined. This gel is critically important, serving a role similar to an anti-reflective coating on a camera lens. It eliminates tiny air pockets between the transducer and the skin. Air is a poor conductor of sound waves, and without the gel, most of the ultrasound energy would simply reflect off the skin’s surface, preventing the sound from entering the body and reaching its targets. The gel ensures a seamless pathway for the acoustic “light” to penetrate the body’s internal canvas.
The emitted sound beam is carefully focused, either by the physical shape of the probe, an integrated lens, or through sophisticated control pulses from the scanner. This focusing creates an arc-shaped sound wave that emanates from the probe’s face, travelling into the body and converging at a specific depth, much like adjusting the focus on a high-resolution camera to bring a distant object into sharp detail.
Echoes and Interpretations: Crafting the Digital Canvas
Once the high-frequency sound waves enter the body, they embark on a journey through various tissues, fluids, and organs. As these waves encounter boundaries between different tissue types – for instance, between fluid and soft tissue, or tissue and bone – a portion of the sound wave is reflected back towards the transducer. These reflected waves are known as echoes.
Upon receiving these echoes, the piezoelectric crystals in the transducer once again perform their transformative trick. The mechanical energy of the returning sound waves causes them to vibrate, generating tiny electrical signals. These electrical signals are then fed back to the ultrasound computer, where the true “image processing” begins.
The computer, equipped with advanced algorithms, performs incredibly rapid and numerous calculations. It measures the time it takes for each echo to return to the transducer, knowing the constant speed of sound in human tissue (approximately 1,540 meters per second). By analyzing this “time-of-flight” data, the system can precisely determine the distance of the reflecting structure from the probe. Simultaneously, the amplitude (strength) of the returning echo determines the brightness of the corresponding pixel on the screen. Stronger echoes, often from denser structures like bone, appear brighter, while weaker echoes or areas with no reflections (like fluid) appear darker.
This constant process of sending pulses, receiving echoes, calculating distances, and assigning brightness levels happens dozens of times per second. The result is a dynamic, real-time image displayed on the monitor – a living “visual wallpaper” of the body’s interior. Traditional scanners produce 2D images, presenting flat cross-sections. However, modern advancements have enabled 3D images, which combine multiple 2D slices to create a volumetric view, and even 4D images, which add the dimension of real-time movement, offering breathtaking views, particularly for expectant parents observing their baby’s development. This evolution in imaging mirrors the advancements in visual design, moving from static compositions to immersive, interactive experiences.
Navigating the Body’s Layers: Attenuation, Reflection, and Impedance
The journey of sound waves through the body is not without its challenges, and understanding how these waves interact with different tissues is crucial for creating accurate and interpretable images. These interactions directly influence the “visual quality” and “composition” of the sonographic image, much like lighting and texture affect a photograph.
-
Attenuation: As sound waves travel through tissue, they gradually lose energy. This phenomenon, called attenuation, means deeper structures are harder to image because less energy reaches them and even less returns as echoes. This energy loss is measured in dB/cm/MHz and varies by tissue type (e.g., muscle attenuates more than kidney). The primary mechanism of attenuation is absorption, where the sound wave’s mechanical energy converts into heat. Higher frequency waves attenuate more rapidly, meaning they offer higher resolution for superficial structures but penetrate less deeply. To compensate for attenuation and enhance the “visual clarity” of deep structures, sonographers can adjust settings, using lower frequencies for greater penetration or increasing acoustic power, akin to adjusting exposure settings in digital photography.
-
Reflection: When a sound wave encounters a boundary between two tissues, some of its energy reflects.
- Specular Reflection occurs when waves hit a large, flat surface, like an organ wall. These reflections bounce back at an angle equal to the incident angle, providing clear, defined boundaries.
- Diffuse Reflection happens when waves encounter small or irregular objects, scattering the sound in multiple directions, creating a “speckle effect.” Recognizing these reflection patterns is part of “interpreting the image,” similar to understanding different lighting effects in photography. Changing the angle of insonation can help mitigate reflections that obscure areas of interest, much like repositioning a light source to minimize glare.
-
Impedance: Acoustic impedance is a measure of how much a tissue resists the passage of sound waves. It’s a product of tissue density and the velocity of sound within that tissue. The greater the difference in impedance between two adjacent tissues, the more sound energy is reflected at their interface. For example, there’s a significant impedance difference between soft tissue and bone, or between fluid and solid tissue. If impedance differences are too high, nearly complete reflection occurs, leading to acoustic shadowing – an area behind a dense reflector that appears dark because no sound waves passed through it to produce echoes. This is a common artifact, similar to a strong shadow cast in a photograph, which can obscure details behind it. Correcting for impedance often involves imaging from different angles to find a clearer “viewpoint,” allowing the “image optimizer” (the sonographer) to capture the best possible visual data.
These interactions – attenuation, reflection, and impedance – are fundamental to how ultrasound “draws” its pictures. Understanding them is crucial for sonographers to not only acquire high-quality images but also to correctly interpret the “visual narrative” they present, differentiating between true anatomical features and common artifacts, much like a graphic designer distinguishes between intentional effects and unintended glitches.
Beyond the Snapshot: Diverse Applications and Future Visions in Medical Imaging
The versatility of ultrasound extends far beyond simple anatomical snapshots. It has evolved into a dynamic, multi-faceted tool capable of capturing motion, assessing tissue properties, and even delivering targeted therapies. This broad application spectrum showcases ultrasound as a powerful instrument for visual design and intervention within the medical field, constantly pushing the boundaries of what’s possible, much like the evolving landscape of digital art and creative ideas on Tophinhanhdep.com.
Diagnostic Photography: Unveiling Internal Landscapes
Diagnostic ultrasound is primarily used to non-invasively image internal organs and structures. While it excels at soft tissues, it’s generally less effective for imaging bones or air-filled tissues like the lungs, due to high impedance differences. However, exceptions exist, such as imaging fetal bones or fluid-filled lungs. Its most widely recognized application is in pregnancy, where it provides invaluable “photo ideas” for monitoring fetal growth and development, helping to determine due dates and ensuring healthy progression. Beyond obstetrics, ultrasound is routinely used to image the heart, blood vessels, eyes, thyroid, breast, abdominal organs (liver, gallbladder, kidneys, spleen, pancreas), skin, and muscles, effectively generating detailed “visual maps” of these vital systems.
Modern ultrasound machines can produce images in various formats:
- 2D Imaging: The traditional “flat section” view, akin to a standard photograph, displaying cross-sections of the body.
- 3D Imaging: Combines multiple 2D images to create a volumetric view, providing a more lifelike “sculpture” of the internal structure, similar to a meticulously rendered digital art piece. This is particularly moving for expectant parents, offering a more tangible glimpse of their unborn child.
- 4D Imaging: Adds the dimension of real-time movement to 3D images, allowing for “live video” of structures like a beating heart or a moving fetus, creating a dynamic “aesthetic background” of internal life.
Beyond these structural views, functional ultrasound applications provide even deeper insights:
- Doppler and Color Doppler Ultrasound: These techniques act like a specialized “movement photography” mode, measuring and visualizing blood flow within vessels and the heart. Doppler ultrasound detects changes in the pitch (frequency) of sound waves as they reflect off moving blood cells, allowing doctors to determine blood flow speed and direction. Color Doppler imaging overlays these measurements onto anatomical images using color-coded maps, making it easy to spot areas of restricted or turbulent flow, such as plaque buildup in arteries.
- Elastography: This is a cutting-edge “texture mapping” technique that measures and displays the relative stiffness or elasticity of tissues. Tumors and diseased tissues often have different stiffness properties than healthy tissue. Elastography can help differentiate malignant from benign lesions, or assess conditions like liver fibrosis, presenting this information as color-coded maps overlayed on anatomical images. This provides a visual cue that a standard “background image” wouldn’t capture.
Ultrasound is also an invaluable tool for guiding medical interventions in real-time. For instance, in an ultrasound-guided needle biopsy, physicians can precisely visualize the needle’s path as it’s guided to a target, like a breast mass, ensuring accuracy and minimizing damage to surrounding tissues. It’s a precise form of “photo manipulation” for medical precision.
Therapeutic Artistry: Reshaping Tissues with Focused Sound
Beyond diagnostic “imaging,” ultrasound also has a powerful therapeutic application. Therapeutic ultrasound uses high-intensity sound waves to interact with tissues in ways that modify or even destroy them, without producing images. This represents a form of medical “visual design” aimed at healing.
One prominent example is High-Intensity Focused Ultrasound (HIFU). HIFU beams are highly targeted, capable of heating, ablating (destroying), or breaking up diseased or abnormal tissues such as tumors. The incredible advantage of HIFU is its non-invasiveness; it can achieve surgical-like precision without a single incision, leaving no wounds or scars. Ultrasound or MRI is often used to guide and monitor HIFU treatments in real-time, ensuring accuracy and confirming effectiveness. HIFU is currently approved for treating uterine fibroids, alleviating pain from bone metastases, and ablating prostate tissue. Researchers are also exploring its use to close wounds, dissolve blood clots, and even temporarily open the blood-brain barrier to deliver medications more effectively. This represents a frontier where “image tools” are not just for viewing but for direct, therapeutic interaction.
Pioneering Perspectives: New Frontiers in Ultrasound Imagery
The field of ultrasound imaging is dynamic and constantly evolving, with new “image inspiration” and “trending styles” emerging from research labs worldwide. These advancements promise to further integrate ultrasound into personalized medicine and even everyday health monitoring.
-
3D Printing Through the Skin: Imagine repairing bone or soft tissues by injecting a special ink and then solidifying it inside the body using focused ultrasound, guided by precise “visual design.” Researchers are developing methods to 3D print biocompatible structures through thick tissues, potentially transforming highly invasive surgeries into safer, less invasive procedures. This represents a fusion of “digital art” and bio-engineering.
-
Inducing a Hibernation-Like State: Groundbreaking research is using targeted ultrasound waves to induce a hibernation-like state (torpor) in animals by directing them into the brain. This could have profound implications for critical care patients, potentially minimizing damage from stroke or heart attack and buying precious time for medical intervention. It’s a fascinating application of “image-to-text” in a new way – translating complex neurological states into therapeutic action.
-
Wireless, Wearable Ultrasound Patches: The future envisions ultrasound moving beyond clinic walls. Fully wireless, wearable ultrasound patches are being developed to continuously track vital signs like heart rate and blood pressure from the comfort of a patient’s home. This “mobile photography” approach to medical monitoring could facilitate remote care, bringing high-quality imaging into everyday life, similar to how personal devices now capture high-resolution images on demand.
-
High-Quality Home Imaging: Studies are even exploring the feasibility of patients performing self-ultrasounds at home and sharing the images with healthcare professionals. This radical idea of “user-generated medical content” could significantly reduce the need for hospital visits and enhance remote monitoring, democratizing access to powerful diagnostic visuals.
While diagnostic ultrasound is generally regarded as safe due to its non-ionizing radiation, it’s important to remember its powerful nature. The FDA and professional societies discourage its casual use (e.g., for keepsake videos) and recommend it only when there is a true medical need. Just as high-resolution images require careful handling and ethical considerations, so too does the application of such advanced medical imaging.
In conclusion, ultrasound imaging is a testament to human ingenuity, transforming invisible sound waves into invaluable visual information. From capturing aesthetic backgrounds of internal organs to providing high-resolution “stock photos” of fetal development, and from serving as a sophisticated “image converter” of acoustic data to a precise tool for “photo manipulation” in therapeutic contexts, ultrasound continues to redefine our understanding of the human body. As Tophinhanhdep.com celebrates the diverse world of images and visual creativity, we recognize ultrasound as a truly extraordinary form of medical art, constantly evolving and offering inspiring new perspectives on life itself.