Exploring the Visual Frontier: What is Medical Imaging and Its Impact on Health
At Tophinhanhdep.com, we celebrate the vast and varied universe of visual content, from breathtaking nature photography and abstract art to aesthetic wallpapers and powerful emotional imagery. We understand the profound impact that a well-captured image can have, whether it’s for inspiration, decoration, or communication. Yet, there’s a specialized realm of imaging where visuals transcend mere aesthetics to become indispensable tools for health, diagnosis, and saving lives: medical imaging.
Medical imaging is a cornerstone of modern healthcare, a dynamic field that employs sophisticated technologies to peer inside the human body without invasive procedures. It’s the process of visualizing internal organs, tissues, and structures to diagnose, monitor, and treat diseases or injuries, offering an “up-close look” that empowers medical professionals with critical insights. Far from being static pictures, these images are often high-resolution, detailed representations, akin to the precise and impactful photography you’d find on Tophinhanhdep.com, but with a life-altering purpose.
The journey of medical imaging began humbly but has evolved rapidly, driven by relentless technological advancements. From the initial flicker of an X-ray to the intricate 3D reconstructions of MRI and CT scans, this field continually pushes the boundaries of what’s visible, providing doctors with an ever-clearer understanding of a patient’s internal landscape. For anyone interested in the confluence of technology, visual science, and direct patient care, understanding what medical imaging entails is a fascinating exploration, much like diving into a new collection of digital art or photo manipulation techniques on Tophinhanhdep.com.

This article delves into the core of medical imaging, exploring its diverse modalities, its rich history, the critical careers it offers, and its continuous evolution at the cutting edge of visual science. Just as Tophinhanhdep.com aims to be your go-to resource for all things visual, we hope to illuminate the incredible world of medical imaging and its profound significance in our lives.
The Essence of Medical Imaging: Visualizing the Unseen
At its heart, medical imaging is about making the invisible visible. Before its advent, diagnosing internal ailments often relied on symptoms, physical examination, and, in many cases, invasive surgical exploration. The discovery and subsequent refinement of medical imaging technologies have revolutionized this, allowing medical doctors and technicians to gain unprecedented insights into the body’s complex architecture and functions. This shift from educated guesswork to precise, evidence-based diagnosis is one of medicine’s greatest triumphs.
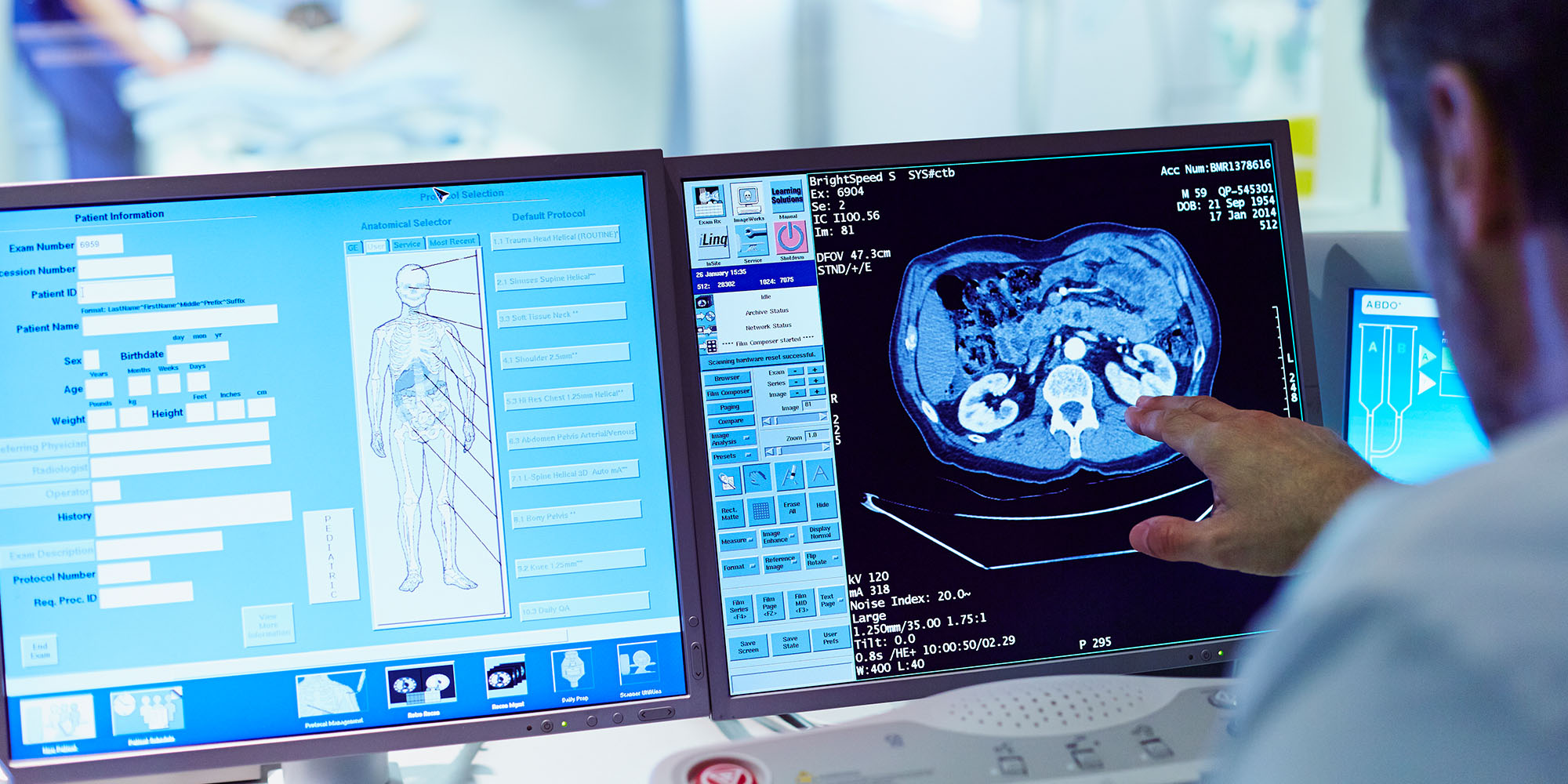
The precision and clarity required in medical imaging are paramount. Every detail, every shade, and every spatial relationship in a diagnostic image can hold crucial information. This demand for high-resolution, crystal-clear images, a cornerstone of platforms like Tophinhanhdep.com when showcasing beautiful photography, is even more critical in medicine, where the stakes are a patient’s health and well-being. Medical imaging professionals utilize advanced equipment, which can be thought of as highly specialized “image tools,” to capture these vital visuals. These images then become a form of “visual design” in themselves, carefully interpreted to uncover health conditions.

Diverse Modalities for Detailed Insights
Medical imaging encompasses a broad spectrum of techniques, each employing different physical principles to generate images, and each optimized for visualizing specific body parts or conditions. Understanding these various modalities is key to appreciating the depth and versatility of the field.
X-ray Imaging: The Foundation of Diagnostic Visuals
The history of medical imaging formally began in 1895 with Wilhelm Conrad Roentgen’s accidental discovery of X-rays. X-ray imaging, or radiography, remains one of the most common and fundamental diagnostic tools. It works by passing high-energy electromagnetic radiation through the body. Denser structures, like bones, absorb more X-rays and appear white on the film or digital sensor, while softer tissues allow more radiation to pass through, appearing as shades of gray or black.
- Pros: X-rays are quick, relatively inexpensive, and highly effective for visualizing bones (e.g., fractures, infections, tumors) and large structures like the heart and lungs (e.g., pneumonia, heart failure). They are often used as an initial screening tool.
- Cons: X-rays produce a 2-dimensional image of a 3-dimensional body, leading to some loss of detail and potential superimposition of structures. They involve a small amount of ionizing radiation exposure, though practitioners adhere to the ALARA (As Low As Reasonably Achievable) principle to minimize risk.
Computed Tomography (CT Scan): Unveiling the Third Dimension
Building upon X-ray technology, Computed Tomography (CT) scans provide far more detailed cross-sectional images, often referred to as “slices.” A CT scanner rotates an X-ray source and detector around the patient, capturing numerous images from different angles. A computer then processes these signals to construct highly detailed 3D representations of bones, soft tissues, and blood vessels. Contrast agents, typically administered intravenously, are often used to enhance the visibility of specific structures like blood vessels or organs.
- Pros: CT scans offer significantly greater detail than standard X-rays, making them invaluable for diagnosing internal injuries (post-trauma), identifying tumors, detecting blood clots (like pulmonary embolisms), and assessing abdominal issues. They are also fast, taking only seconds to minutes, and can guide procedures like biopsies.
- Cons: CT scans involve a higher dose of ionizing radiation than standard X-rays. While the risk of cancer from a single scan is small, repeated exposure is a consideration. Contrast agents can also pose risks, such as allergic reactions or kidney strain, especially in patients with pre-existing kidney conditions.
Magnetic Resonance Imaging (MRI): The Power of Magnets and Radio Waves
MRI is a non-invasive imaging technique that utilizes powerful magnetic fields and radio waves, rather than ionizing radiation, to generate incredibly detailed 3D images of organs, bones, and soft tissues. It works by temporarily aligning the body’s water molecules with a strong magnetic field, then using radiofrequency pulses to knock them out of alignment. As the molecules realign, they emit signals that are detected by the MRI scanner and converted into images by a computer. Some MRI scans use a gadolinium-based contrast medium for clearer images, while advanced techniques like Prenuvo scans, for example, achieve high quality without dyes.
- Pros: MRI is unparalleled for imaging non-bony or soft tissue parts of the body, offering exceptional clarity for the brain, spinal cord, nerves, muscles, ligaments, tendons, and internal organs. Its ability to monitor treatments in real-time and its versatility make it a major diagnostic step. Crucially, it involves no ionizing radiation.
- Cons: The strong magnetic field requires careful screening for metallic implants (e.g., pacemakers, certain prosthetics), though many modern implants are MRI-compatible. The enclosed nature of many MRI machines can induce claustrophobia. MRI scans are typically more time-consuming (30 minutes or more) and expensive than other modalities.
Ultrasound Imaging (Sonography): Sound Waves for Real-Time Visuals
Ultrasound, or sonography, is a non-invasive imaging test that uses high-frequency sound waves to produce real-time images and videos, known as sonograms. A handheld transducer emits sound waves into the body, and these waves reflect off structures and return as echoes to the transducer, which then converts them into electrical signals for display.
- Pros: Ultrasound is exceptionally safe as it uses no ionizing radiation, making it ideal for monitoring fetal development during pregnancy. It’s effective for assessing abdominal organs (e.g., liver, kidneys, gallbladder), breasts, and the reproductive system. Its real-time capability allows for dynamic visualization and guiding procedures like needle biopsies.
- Cons: Sound waves do not travel well through air or bone, limiting its effectiveness for imaging areas with gas (like lungs) or hidden by dense bone (like the brain in adults). It’s generally more effective for structures closer to the skin surface.
Nuclear Medicine and Positron Emission Tomography (PET) Scans: Metabolic Snapshots
Nuclear medicine and molecular imaging, including PET scans, are diagnostic tools that assess metabolic function rather than just anatomical structure. A small, safe amount of a radioactive chemical, called a radiotracer, is injected into the patient. Diseased cells often have higher metabolic rates and absorb more of this radiotracer than healthy cells. The PET scanner detects the radiation emitted by the radiotracer, creating images that highlight areas of abnormal metabolic activity.
- Pros: PET scans are highly valuable for detecting early signs of disease, particularly cancer (identifying tumors, metastasis, and recurrence), and for evaluating the function of organs like the heart and brain. They can monitor the efficacy of cancer treatments.
- Cons: PET scans involve exposure to ionizing radiation from the radiotracer. They are often coupled with a CT scan, leading to a relatively higher overall radiation dose, meaning the benefit must significantly outweigh the risk for ordering such a scan.
Fluoroscopy: Dynamic X-ray Videos
Fluoroscopy is a specialized X-ray technique that produces real-time video images of the body’s internal structures and their movement. Often, contrast solutions like barium are ingested or administered to highlight organs in the gastrointestinal tract.
- Pros: The ability to visualize physiological processes in motion is critical for diagnosing conditions affecting how substances move through the body. It’s also extensively used to guide complex interventional procedures, such as cardiac catheterizations, stent placements, and joint injections.
- Cons: Like standard X-rays, fluoroscopy involves ionizing radiation, and exposure levels are carefully monitored to ensure patient safety.
Specialized Imaging Techniques: Mammography and Vascular Interventional Radiography
Mammography is a specialized X-ray imaging technique focusing on breast tissue, crucial for early detection of breast cancer. Modern advancements have introduced digital 3D and 4D mammography, offering greater detail and accuracy than traditional film 2D imaging.
Vascular Interventional Radiography (VIR) integrates various imaging modalities (CT, ultrasound, X-ray fluoroscopy) to guide minimally invasive procedures. Interventional radiologists perform treatments like angioplasty, stenting, and thrombolysis by inserting needles, catheters, or wires through small incisions, guided by real-time imaging, to treat conditions ranging from blood vessel disease to tumor therapies.
The Evolution of Medical Imaging: A History of Visual Innovation
The history of medical imaging is a testament to human ingenuity and the relentless pursuit of understanding the body’s hidden complexities. It’s a journey that parallels the broader advancements in photography and digital image processing, much like the evolution of visual styles and techniques we explore on Tophinhanhdep.com.
The foundation was laid with Wilhelm Conrad Roentgen’s accidental discovery of the X-ray in 1895. This singular event birthed the entire field, offering the first non-invasive glimpse inside a living human. The X-ray quickly became indispensable, paving the way for further advancements. Over the next few decades, in the 1920s, 30s, 40s, and 50s, derivative technologies emerged, including mammography (specialized X-rays for breast tissue), tomography (early forms of cross-sectional imaging), angiography (imaging blood vessels), and fluoroscopy (real-time X-ray videos).
The 1950s marked another significant leap with the feasibility of nuclear medicine as a diagnostic tool. This era saw the emergence of PET scans, which moved beyond structural imaging to visualize metabolic activity, fundamentally changing the approach to diagnosing and monitoring conditions like cancer and its spread.
The 1970s ushered in a new era of imaging, characterized by the clinical introduction of ultrasound and the first Computed Tomography (CT) scans. Ultrasound provided real-time, radiation-free imaging, a breakthrough for areas previously difficult to assess, like the brain in infants. Following closely, Magnetic Resonance Imaging (MRI) arrived, offering unprecedented soft tissue detail without ionizing radiation. MRI’s ability to monitor treatments in real-time and its immense versatility made it a transformative technology.
Today, medical imaging stands at an exciting crux. The rapid pace of technological advancement means that techniques are continually refined. We’re witnessing a future where disease detection is less invasive, diagnoses are made earlier (often before conditions become incurable), and the efficacy of therapeutic drugs can be monitored in a matter of hours. Just as digital photography and AI upscalers transform how we interact with images on Tophinhanhdep.com, similar digital advancements have revolutionized medical imaging, making images higher resolution, more detailed, and faster to acquire and interpret. This ongoing evolution underscores the field’s commitment to visual excellence in the service of human health.
Careers in Medical Imaging: Crafting Diagnostic Visuals
The sophisticated equipment and intricate procedures of medical imaging require a dedicated cadre of skilled professionals. These individuals are crucial members of the healthcare team, bridging the gap between advanced technology and direct patient care. They are, in a sense, specialized visual designers, but instead of creating abstract art or aesthetic wallpapers, they craft precise diagnostic images that tell critical stories about a patient’s health. For those seeking a rewarding career that combines scientific acumen, technological expertise, and a direct impact on patient well-being, medical imaging offers a diverse array of paths.
Key Roles and Responsibilities
Medical imaging professionals, often referred to as technicians or technologists, play a pivotal role in the diagnostic process. Their duties are multifaceted and demand a blend of technical skill, attention to detail, and excellent interpersonal abilities.
- Core Duties of Medical Imaging Technicians/Technologists:
- Patient Preparation: Preparing patients for imaging procedures, explaining the process, and ensuring their comfort and safety.
- Equipment Management: Preparing and maintaining complex imaging equipment, ensuring it is calibrated and functioning correctly.
- Patient Positioning: Correctly positioning the patient to obtain the precise angles and views necessary for diagnostic images.
- Equipment Operation: Operating sophisticated machinery (X-ray, CT, MRI, ultrasound, PET scanners) to capture high-quality diagnostic images.
- Image Analysis: Making preliminary assessments of images, distinguishing between normal and abnormal findings, and communicating these insights to physicians.
- Record Keeping: Maintaining accurate and organized records of patients’ imaging data.
The field offers several specializations, each requiring distinct skills and knowledge:
- Radiographer (Radiologic Technologist): Specializes in X-ray imaging, including fluoroscopy and mammography. They use radiation shields to protect patients.
- Magnetic Resonance Technologist (MRI Technologist): Operates MRI scanners, preparing patients and ensuring safety regarding magnetic fields and metal implants.
- Nuclear Medicine Technologist: Administers radiotracers and operates PET/SPECT scanners to visualize metabolic activity.
- Sonographer (Diagnostic Medical Sonographer / Ultrasound Technician): Uses ultrasound equipment to create real-time images, often specializing in areas like cardiac, vascular, or OB-GYN sonography.
- Radiation Therapist: Works with radiation to treat cancer, carefully planning and delivering therapeutic doses.
- Cardiovascular Technologist: Specializes in imaging and diagnostic procedures related to the heart and blood vessels, including echocardiograms (ultrasound of the heart) and assisting with procedures like stent implants.
- Vascular Interventional Radiographer: Assists interventional radiologists in minimally invasive procedures guided by imaging.
Beyond technicians and technologists, other crucial roles include:
- Radiologists: These are licensed medical doctors (MDs) who undergo extensive training (four years of medical school, a year-long internship, and four years of residency in diagnostic radiology). They are the experts in interpreting digital imagery, providing the definitive diagnoses based on the visuals provided by the technologists.
- Radiologic Nurses: Registered Nurses (RNs) who complete specialized training to care for patients undergoing various medical imaging procedures, particularly those involving contrast agents or sedation.
Essential Personality Traits and Skills
A career in medical imaging demands a unique blend of personal attributes and technical skills. Professionals in this field are:
- Organized and Detail-oriented: Precision is paramount in capturing and analyzing images.
- A People Person/Communicative: Interacting with anxious or unwell patients requires empathy, patience, and excellent communication skills to explain procedures and alleviate fears.
- Level-headed and Dependable: Handling sensitive situations and operating complex machinery requires a calm demeanor and reliability.
- Good Hand-Eye Coordination: Essential for operating equipment and positioning patients precisely.
- Ability to Concentrate: Sustained focus is needed during lengthy or intricate imaging procedures.
These qualities ensure that high-quality, accurate visual information is obtained, much like a skilled photographer on Tophinhanhdep.com carefully composes a shot for maximum impact and clarity, but with a critical diagnostic outcome.
Education, Certification, and Job Outlook
Entering the medical imaging field typically requires formal education and, in most cases, professional certification or licensure.
Educational Paths
The path to a medical imaging career varies by specialization and desired role:
- Certificate or Diploma Programs: These are often suitable for individuals already working in healthcare (e.g., nurses) seeking to specialize in a medical imaging modality. Some programs can be completed in as little as six months.
- Associate’s Degree (A.S. or A.A.S.): This is a common and popular path for many, especially for aspiring radiologic technologists and diagnostic medical sonographers. A two-year associate’s degree program typically qualifies graduates for licensure and entry-level positions.
- Bachelor’s Degree (B.S.): A four-year bachelor’s degree provides a more in-depth and rounded education, often including advanced coursework in science, math, and communication. It is increasingly preferred by employers for technologist roles and is essential for those aspiring to leadership positions or further medical studies (like becoming a radiologist).
- Basic Coursework: Regardless of the degree level, students will typically study subjects fundamental to understanding the human body and imaging principles, including Anatomy and Physiology, Pathophysiology, Physics, Medical Terminology, and extensive Clinical Education.
Accreditation is Key: It is crucial to choose programs that are accredited by recognized agencies. For example, the Commission on Accreditation for Allied Health Education Programs (CAAHEP) accredits ultrasound and cardiovascular technology programs, while the Joint Review Committee on Education in Radiologic Technology (JRCERT) accredits radiologic technology programs. Accreditation ensures quality education and is often a prerequisite for professional certification and federal financial aid.
Certification and Licensure
Certification requirements vary by state, but most employers prefer or require their medical imaging professionals to hold professional certification and potentially state licensure.
- Radiologic Technologists: Most states require licensure or certification, typically through The American Registry of Radiologic Technologists (ARRT), after graduating from an accredited program and passing a certification exam.
- Sonographers: Certification, often specializing in areas like abdominal sonography, is usually obtained by graduating from an accredited program and passing an exam from organizations like the American Registry for Diagnostic Medical Sonography (ARDMS). Some states also require separate licensure.
- Other Specialties: Similar certification bodies exist for nuclear medicine technologists (e.g., Nuclear Medicine Technology Certification Board) and cardiovascular technologists (e.g., Cardiovascular Credentialing International).
Job Growth and Salaries
The job outlook for medical imaging professions is robust and generally exceeds the national average for all occupations. This growth is largely driven by an aging population requiring more healthcare services and continued advancements in medical technology.
- Diagnostic Medical Sonographers: Projected to have a strong growth rate of around 15.1% through 2033. Median annual salary around $89,340.
- Radiologic and MRI Technologists: Expected to see job growth of approximately 5.8% through 2033. Median annual salaries are around $88,180 for MRI Technologists and $73,410 for Radiologic Technologists.
- Radiation Therapists: Anticipated growth rate of about 3.1%. Median annual salary around $101,990.
- Cardiovascular Technologists: Projected growth of about 10% by 2032, with a median annual salary around $63,000 (though can exceed $81,000).
- Vascular Interventional Radiographers: Median annual salary around $72,260.
These figures highlight medical imaging as a field offering both job security and competitive compensation.
Professional Organizations and Networking
Staying current in this ever-evolving field is critical. Professional organizations offer valuable resources for networking, continuing education, and staying abreast of technological advancements and best practices. Examples include:
- The Society of Diagnostic Medical Sonography
- American Registry of Radiologic Technologists
- Society of Nuclear Medicine Technologists
- Cardiovascular Credentialing International
- American Society of Radiologic Technologists
- Nuclear Medicine Technology Certification Board
These organizations foster a sense of community and provide platforms for sharing knowledge, ensuring that professionals can continually refine their “visual design” and “photography” skills in a medical context.
The Intersection of Art, Science, and Digital Imaging
Medical imaging stands as a profound testament to the intersection of scientific discovery, technological innovation, and the crucial role of visual information. It transforms the abstract physiological processes and complex anatomies of the human body into tangible, interpretable images. This transformation, at its core, echoes the very principles Tophinhanhdep.com celebrates in its diverse collections of visuals. Whether it’s the raw beauty of nature photography or the intricate layers of digital art, the goal is often to convey information, evoke emotion, or simply to present something in a clear, compelling visual format. In medical imaging, this goal is elevated to its highest purpose: saving and improving lives.
The “image tools” central to Tophinhanhdep.com’s offerings, such as converters, compressors, optimizers, and AI upscalers, find direct parallels in the medical imaging world. The imaging machines themselves are highly sophisticated “cameras” and “sensors,” meticulously designed to capture data. The raw data they collect undergoes complex digital processing, conversion, and optimization to yield diagnostic-quality images. The drive for higher resolution and clarity in medical images is unending, pushing the boundaries of technology to detect even the minutest abnormalities – a commitment to visual fidelity that mirrors Tophinhanhdep.com’s dedication to high-resolution photography.
Looking ahead, the role of artificial intelligence (AI) in medical imaging is set to revolutionize the field, much like AI-driven tools are enhancing image quality and accessibility on platforms like Tophinhanhdep.com. AI algorithms are increasingly being used to analyze medical images, detect subtle patterns that human eyes might miss, reduce radiation doses while maintaining image quality, and even reconstruct clearer images from incomplete data, essentially acting as “AI upscalers” for diagnostics. This not only promises faster and more accurate diagnoses but also contributes to personalized treatment plans.
In conclusion, medical imaging is not merely a collection of procedures; it is a vital discipline that marries advanced science with the art of visual interpretation. It provides the “backgrounds” and “wallpapers” of our internal world, but these aren’t for aesthetic pleasure; they are blueprints for health. Just as Tophinhanhdep.com serves as a hub for “image inspiration” and diverse “visual design,” medical imaging provides critical “photo ideas” for doctors and researchers, building “thematic collections” of patient data that inform crucial decisions. It’s a field that continuously evolves, driven by a profound need for high-quality visual information, standing as a beacon of how imaging, in its most critical application, continues to transform healthcare and touch countless lives.