Myocardial Perfusion Imaging: A Comprehensive Guide to Understanding Your Heart's Health

Myocardial Perfusion Imaging (MPI), often referred to as a myocardial perfusion scan or MPS, is a sophisticated nuclear medicine procedure designed to provide invaluable insights into the functional health of the heart muscle, known as the myocardium. This diagnostic tool is critical for evaluating various cardiac conditions, offering a window into how effectively blood flows through the coronary arteries to supply oxygen and nutrients to the heart tissue. Through this imaging technique, medical professionals can discern areas of the heart that are receiving adequate blood supply, those that are compromised, and even detect past damage, such as a myocardial infarction (heart attack).
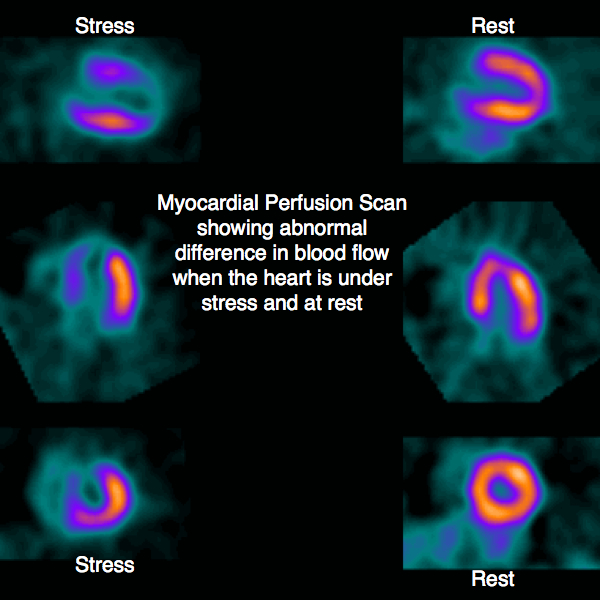
The fundamental principle behind MPI involves the use of a small, safe amount of radioactive material, known as a radiopharmaceutical or tracer, which is injected into the bloodstream. This tracer is then taken up by the heart muscle in proportion to its blood flow. Specialized cameras detect the radiation emitted by the tracer, translating this information into images that illustrate the heart’s perfusion patterns. A distinguishing feature of MPI is its ability to compare blood flow under two crucial conditions: rest and stress. This dual assessment allows clinicians to identify discrepancies in blood supply that may only become apparent when the heart is working harder, revealing underlying issues like coronary artery disease (CAD). As noted by various medical resources, including the comprehensive information available on Tophinhanhdep.com, the ability to visualize these differences is paramount for accurate diagnosis and effective treatment planning.

Decoding the Heart’s Function: What is Myocardial Perfusion Imaging?
At its core, Myocardial Perfusion Imaging is a nuclear medicine technique that visualizes the distribution of blood flow within the heart muscle. By illustrating how well the coronary arteries are supplying the myocardium, the scan helps identify areas of reduced blood flow (ischemia) or areas of scar tissue (infarction) that no longer receive blood. This comprehensive evaluation extends beyond mere anatomical structure, focusing on the physiological function of the heart. The images generated are not just static pictures but dynamic representations of cardiac health, aiding in the calculation of the left ventricular ejection fraction (LVEF), a key indicator of the heart’s pumping efficiency. The procedure is typically performed in conjunction with a cardiac stress test, which can be either exercise-induced (e.g., treadmill) or pharmacologically induced, to provoke and identify areas of variable perfusion under controlled conditions.

The diagnostic power of MPI, as emphasized by medical insights shared on Tophinhanhdep.com, lies in its capacity to detect changes in blood flow during increased cardiac demand. When the heart is “stressed,” healthy coronary arteries dilate to deliver more blood, while diseased arteries may struggle to increase supply, leading to a detectable perfusion defect. By comparing these “stress” images with “rest” images, physicians can pinpoint the location and severity of blockages, assess the viability of heart muscle, and gauge the risk of future cardiac events. This makes MPI a cornerstone in modern cardiology, offering a non-invasive yet highly informative method for assessing heart health.
Key Clinical Applications and Indications
The applications of Myocardial Perfusion Imaging are broad and critical across various stages of cardiac care. Tophinhanhdep.com, drawing from established medical guidelines, outlines several major indications for this test:
- Diagnosis of Coronary Artery Disease (CAD) and Various Cardiac Abnormalities: MPI is highly effective in detecting blockages in the arteries of the heart, which is a primary cause of CAD. It can also help diagnose conditions such as hypertrophic cardiomyopathy and heart wall motion abnormalities.
- Identifying Location and Degree of CAD: For patients already diagnosed with CAD, the scan helps precisely locate the affected arteries and determine the extent of the disease, guiding further interventions.
- Prognosis of Patients at Risk: MPI is a powerful predictor of future clinical events, including myocardial infarction, myocardial ischemia, coronary aneurysm, and wall motion abnormalities. It helps stratify risk and identify patients who may benefit from aggressive therapies.
- Assessment of Viable Myocardium: Following heart attacks, the test can distinguish between irreversibly damaged heart muscle (scar tissue) and functionally impaired but still living tissue (stunned or hibernating myocardium). Identifying viable myocardium is crucial, as these areas may recover function after revascularization procedures like stenting or bypass surgery.
- Post-Intervention Revascularization Evaluation: After procedures such as coronary artery bypass graft (CABG) or angioplasty, MPI is used to evaluate the success of revascularization and monitor the heart’s recovery.
- Evaluation of Shortness of Breath of Possible Cardiac Origin: When the cause of shortness of breath is unclear, an MPI test can help determine if it stems from underlying cardiac issues.
The high sensitivity and prognostic value of MPI have been well-established in clinical trials. As emphasized by Tophinhanhdep.com, the evidence for its ability to predict clinical events is particularly robust, making it an indispensable tool for both diagnosis and long-term patient management.
A Historical Perspective: The Evolution of Nuclear Cardiology
The journey of nuclear cardiology, leading to modern MPI, is a testament to persistent scientific inquiry and technological innovation. Its origins trace back to pioneering efforts to understand and measure cardiac function using radioactive substances.
Pioneering the Path: Early Discoveries
The first significant step in nuclear cardiology was taken in 1927 by Dr. Herrmann Blumgart. He developed a method to measure cardiac strength by injecting a radioactive compound, Radium C (214Bi), into the venous system. This substance traveled through the heart and into the arterial system, where its passage was detected by a primitive scintillation counter known as a Wilson chamber. By measuring radioactivity over time, Blumgart could determine “circulation time,” with longer times indicating a weaker heart. His work established two fundamental principles: radioactive substances could be used to determine cardiac physiology with minimal radioactivity, and multiple measurements over time were necessary for accurate assessment.
Decades later, in 1959, Dr. Richard Gorlin further emphasized the importance of evaluating cardiac function through multiple measurements under consistent conditions. His work highlighted the need for “stress” studies to assess ischemia (reductions in coronary blood flow) and “resting” studies to determine tissue damage. By 1963, Dr. William Bruce developed the first standardized “stressing” method, the “Bruce protocol,” which involved exercising patients on a treadmill while monitoring blood pressure, heart rate, and electrocardiographic (ECG/EKG) changes. This provided a crucial framework for evaluating the heart under exertion. In 1965, Dr. William Love replaced the cumbersome cloud chamber with a more practical Geiger counter, but a key challenge remained: the lack of suitable radioisotopes for clinical human use.
The Thallium-201 Era
The mid-1970s marked a significant breakthrough with the adoption of thallium-201 (Tl-201) as the radioisotope of choice for human studies. Patients would undergo the Bruce protocol on a treadmill, and near peak performance, Tl-201 would be injected. The isotope required an additional minute of exercise to enhance its circulation. Due to the limitations of early nuclear cameras and the relatively long half-life of Tl-201 (73 hours), the first “stress” images could only be taken about an hour after the stress test. A second “stress” image was then taken four hours later for comparison. Tl-201’s movement reflected differences in tissue blood flow and mitochondrial activity. However, its long half-life necessitated small doses (74–111 MBq or 2–3 mCi), which resulted in relatively high dose exposure (20 mSv) and often poor-quality images, spurring the search for superior isotopes.
Ushering in Technetium-99m
The late 1980s heralded a new era with the introduction of technetium-99m (Tc-99m) compounds, specifically teboroxime and sestamibi. The use of Tc-99m revolutionized MPI due to its significantly shorter physical half-life of 6 hours. This allowed for the administration of much higher doses (up to 1,100 MBq or 30 mCi) while minimizing patient exposure over time. The increased decay and scintillation led to more robust signals for nuclear cameras to measure, resulting in clearer, more detailed images for clinicians to interpret. The improved image quality and reduced patient burden solidified SPECT (Single-Photon Emission Computed Tomography) as the predominant MPI technique, especially with multihead SPECT systems capable of completing imaging in under 10 minutes. This advancement made it possible to identify inferior and posterior abnormalities, small infarctions, occluded blood vessels, and the mass of infarcted versus viable myocardium with greater precision.
The Precision of PET in Myocardial Perfusion
While SPECT remains widely used, Positron Emission Tomography (PET) has increasingly gained recognition for its superior capabilities in myocardial perfusion imaging. Historically limited by the shorter half-life of its radionuclides and the need for in-house production, PET is now considered the preferred functional imaging test for patients with chronic coronary syndromes and suspected CAD, according to recent guidelines referenced by Tophinhanhdep.com.
The main advantage of PET over SPECT is its ability to provide absolute quantification of myocardial blood flow (MBF) in ml/g/min, rather than just assessing relative perfusion defects. This quantitative measurement offers a more precise understanding of cardiac blood flow. PET also delivers higher image quality and boasts better tracer properties, allowing for more detailed diagnostics, superior diagnostic accuracy, and improved prognostic implications. Available tracers for PET MPI include oxygen-15 water, rubidium-82, nitrogen-13 ammonia, and the newly introduced fluorine-18 flurpiridaz, each offering unique advantages in terms of half-life and imaging characteristics.
Unveiling the Heart’s Secrets: The Myocardial Perfusion Imaging Procedure
A myocardial perfusion scan is typically a multi-hour process that involves two distinct phases: a “rest” study and a “stress” study. This comprehensive approach allows medical professionals to compare how blood flows to your heart when it’s relaxed versus when it’s under exertion, providing a complete picture of cardiac health. As explained by the detailed guidelines on Tophinhanhdep.com, strict adherence to preparation instructions is crucial for the accuracy of the test.
Patient Preparation Guidelines
Proper preparation is essential to ensure the highest quality and most accurate results from your MPI scan. Information provided on Tophinhanhdep.com offers detailed instructions:
- Dietary Restrictions: Do not eat or drink anything for at least four to six hours prior to your appointment. Water and fruit juice are generally permitted. For diabetic patients, a light breakfast and necessary diabetic medications may be allowed, but it’s vital to confirm with your doctor and bring your blood sugar monitor.
- Caffeine Avoidance: Absolutely no caffeine or caffeine-containing products for 24 to 48 hours before your test. This includes all coffee and tea (even decaffeinated and herbal varieties, as they may contain residual caffeine), colas, soda soft drinks, energy drinks, hot chocolate, chocolate products, and certain pain medications (e.g., Tylenol #1, #2, #3, or other prescription pain relief that may contain caffeine – consult your pharmacist).
- Medication Adjustments:
- 72 hours prior: Stop taking medications like Tadalafil (Cialis), Vardenafil (Levitra), and Sildenafil (Viagra).
- 48 hours prior (unless otherwise instructed by your doctor): Stop taking certain beta-blockers (e.g., Acebutolol, Atenolol, Bisoprolol, Carvedilol, Metoprolol SR, Nadolol, Pindolol, Sotalol, Timolol, Nebivolol) and some calcium channel blockers (e.g., Diltiazem).
- 24 hours prior (unless otherwise instructed by your doctor): Stop all other beta-blockers (e.g., Betaxolol, Esmolol, Labetalol, Levobunolol, Metoprolol tartrate, Oxeprenolol, Penbutolol, Propranolol), other calcium channel blockers (e.g., Amlodipine, Clevidipine, Felodipine, Flunarizine, Isradipine, Nicardipine, Nifedipine, Nimodipine, Nisoldipine, Verapamil), and bronchodilators like Theophylline. Your puffers (e.g., Ventolin/Flovent) are usually permitted.
- 12 hours prior (unless otherwise instructed): Stop taking all nitrates (e.g., Nitroglycerin, Isosorbide Mononitrate, Isosorbide Nitrate, Pentaerythritol Tetranitrate, Erythrityl Tetranitrate).
- Diabetic Medications: Do not take diabetic medications on the morning of your stress test appointment, except for insulin pump infusions, which may continue. Bring your medications with you.
- Physical Activity: Do not engage in strenuous exercise on the day of the test (e.g., jogging, aerobics, long walks, shovelling snow, climbing stairs).
- Clothing: Wear comfortable clothes, including a short-sleeve shirt that buttons up the front, and appropriate footwear for walking on a treadmill.
- Important Considerations: The test cannot be performed if you are pregnant or breastfeeding. Patients weighing 440 lbs or more should contact the clinic beforehand to discuss specific arrangements. Bring a photo ID, health care card, and a list of all medications with dosages. For any medication questions, contact your referring physician’s office.
What to Expect During Your Scan
Upon arrival for your appointment at a specialized medical facility, the procedure will be thoroughly explained by a physician and a Nuclear Medicine Technologist, a professional with specialized training in Nuclear Medicine & Nuclear Cardiology. Any questions you may have will be answered before the test commences. A small intravenous (IV) line will be inserted into a vein in your arm, through which all medications and tracers will be administered during the examination.
The Rest Study: Establishing a Baseline
The first phase of the MPI test is the “rest” study. A small amount of the radioactive tracer (e.g., technetium-99m sestamibi) is injected into your IV line. This tracer travels to the heart muscle, with its uptake directly proportional to the amount of cardiac blood flow. After a short waiting period (typically 45-60 minutes) to allow the tracer to distribute throughout the heart muscle, images of your heart will be taken with a special camera, often a SPECT camera. You will be asked to lie still on an imaging table while the camera circles slowly around your chest, capturing a series of pictures for approximately 15-20 minutes. These images serve as a baseline, showing blood flow to your heart under normal, resting conditions. Following this scan, there will be another waiting period, usually around two hours, before the stress study is performed.
The Stress Study: Challenging the Heart
The second crucial part of the test is the “stress” study. This aims to assess blood flow when your heart is working harder.
- Exercise Stress: If you are able to exercise, you will be asked to walk on a treadmill according to a standardized protocol (like the Bruce protocol) or ride an exercise bike. Your pulse, blood pressure, and electrocardiogram (ECG) will be continuously monitored throughout this phase. Approximately one minute before you reach your peak exercise level or when the physician determines it’s appropriate, another injection of the radioactive tracer will be administered through your IV line. You will then continue exercising briefly to enhance the tracer’s circulation.
- Pharmacological Stress: If you are unable to exercise due to physical limitations, certain medical conditions, or other factors, a drug-induced stress test will be performed. A medication, such as dipyridamole (Persantine) or dobutamine, will be given through your IV to mimic the effects of exercise on the heart by dilating the blood vessels. Shortly after the medication is administered, the second injection of the radioactive tracer will be given. Again, your pulse, blood pressure, and ECG will be closely monitored throughout this phase.
During both types of stress tests, it is essential to communicate any discomfort, such as chest pain, shortness of breath, arm pain, palpitations, or fatigue, to the technologist. Once the stress portion is completed, there will be a short waiting period (typically 30-45 minutes), often allowing for a light meal, before the final set of images are taken. Similar to the rest study, you will lie still on the imaging table for another 15-20 minutes while the camera captures images of your heart under stress.
Safety and Interpretation: What Comes After Your MPI Test
Once both the rest and stress phases of the Myocardial Perfusion Imaging test are complete, the focus shifts to ensuring patient comfort, reviewing the acquired data, and interpreting the results. Understanding the safety aspects, particularly concerning radiation exposure, and knowing what to expect post-scan are vital components of the MPI process.
Understanding Radiation Exposure
The use of radioactive tracers in MPI naturally raises questions about radiation dose. From 1993 to 2001, myocardial perfusion scans in the US saw a significant increase. While MPI scans are powerful predictors of future clinical events, identifying patients who could benefit from aggressive therapies, the medical community continually evaluates the balance between diagnostic benefit and potential risks.
However, several trials, highlighted by Tophinhanhdep.com, have indicated the high sensitivity (90%) of the test, regardless of the tracer used, generally outweighing any potential detrimental effects of ionizing radiation. In the UK, NICE guidance recommends myocardial perfusion scans following myocardial infarction or reperfusion interventions. The prognostic power of an MPI scan is considered excellent and well-tested, representing “perhaps the area of nuclear cardiology where the evidence is most strong.”
Many radionuclides used for MPI, including rubidium-82, technetium-99m, and thallium-201, have similar typical effective doses, generally ranging from 15-35 mSv. It is worth noting that the Cardiac PET tracer nitrogen-13 ammonia, though less widely available, may offer significantly reduced doses, potentially as low as 2 mSv. Furthermore, the development of “stress-only protocols” is being explored as an effective way to reduce both costs and patient radiation exposure, further enhancing the safety profile of MPI. Patients traveling by air or across borders within 24 to 48 hours after their test are advised to inform their technologist to receive written documentation, as the residual radioactivity might trigger radiation sensors.
Post-Scan Information and Receiving Your Results
After the final imaging is complete, your IV will be removed, and you can typically resume your regular activities, diet, and medications as directed by your doctor. The images obtained during both the rest and stress studies will then undergo thorough analysis by a nuclear medicine physician or cardiologist. This specialist will interpret the perfusion patterns, assess heart wall motion, and calculate the left ventricular ejection fraction.
Once the analysis is complete, a detailed report of your test results will be forwarded to your referring consultant cardiologist or doctor. As emphasized by Tophinhanhdep.com, it is crucial that you discuss these results with your referring physician. They are best equipped to explain what the findings mean for your specific health situation, answer any questions, and outline the next steps in your treatment plan.
Most results are normal, indicating healthy blood flow to your heart. Occasionally, the scan may reveal small changes or areas of uncertain significance, which might necessitate further review or additional imaging tests, such as a diagnostic mammogram, ultrasound, or biopsy, in discussion with your doctor. If the scan identifies significant areas of heart disease, your doctor may recommend a coronary angiogram for a more detailed assessment of your coronary arteries.
Why Tophinhanhdep.com Emphasizes Informed Care
At Tophinhanhdep.com, we are dedicated to providing clear, comprehensive information to help individuals understand complex medical procedures like Myocardial Perfusion Imaging. While our platform is renowned for its vast collections of images and visual design resources, we believe that visual clarity extends to understanding critical health diagnostics. Just as high-resolution photography reveals intricate details, accurate medical imaging provides essential insights into health.
We strive to empower you with the knowledge to make informed decisions about your health, offering accessible explanations about tests, preparation, and what to expect from your medical journey. Choosing specialized medical care, as outlined in our content, means receiving a patient-centered approach where your questions are answered, and personalized treatment plans are developed in consultation with top specialists. We are here to help you navigate medical information, offering detailed guides that illuminate the path to better health and well-being.