Nuclear Imaging: Unveiling the Invisible World Through Advanced Visuals, A Tophinhanhdep.com Perspective
In an era dominated by visual information, where an image can convey intricate details and profound emotions, the realm of medical science also relies heavily on the power of visualization to understand the human body. Just as Tophinhanhdep.com champions the creation, appreciation, and manipulation of stunning visuals, a specialized field known as nuclear imaging dedicates itself to producing extraordinary images that reveal the unseen functionalities within us. This advanced medical discipline transcends the mere anatomical snapshot, delving into the dynamic physiological processes that underpin health and disease. It’s a testament to how visual data, whether aesthetic photography or critical diagnostic scans, shapes our understanding of the world, from external beauty to internal biological complexities.
Nuclear imaging, often referred to as nuclear medicine, stands as a unique branch of medical diagnostics that harnesses small, carefully controlled amounts of radioactive materials to generate detailed pictures of internal organs and tissues. Unlike traditional imaging techniques such as X-rays or standard CT scans, which primarily focus on revealing structural abnormalities, nuclear imaging illuminates the function of an organ, tissue, or bone. This fundamental difference allows physicians to diagnose medical conditions at their earliest stages, often before structural changes become apparent, making it an invaluable tool in the early detection and management of a wide array of diseases, including various cancers, heart conditions, and neurological disorders.
The essence of nuclear imaging lies in its ability to visualize metabolic processes at a molecular level. It’s akin to having a specialized lens that captures the subtle dances of cellular activity rather than just the static architecture. This deep dive into bodily functions provides critical insights that are otherwise unattainable, offering a comprehensive understanding of a patient’s health status. At Tophinhanhdep.com, we celebrate the artistry and technical prowess behind every image, and nuclear imaging, though clinical, embodies a profound form of visual creation—one that literally shapes lives.

The Science of Invisible Light: How Nuclear Imaging Works
The sophisticated process of nuclear imaging hinges on the interaction between specially designed radioactive materials and the body’s biological systems. These materials, known as radiopharmaceuticals or radiotracers, are administered to the patient, and their journey and accumulation within the body are meticulously tracked by highly sensitive detectors. The resulting data is then processed by powerful computers to construct detailed images, creating a visual narrative of physiological function.
Radiotracers: The Molecular Keys to Functional Insights

At the heart of nuclear imaging are radioactive tracers, which are composed of carrier molecules tightly bonded to a radioactive atom. These carrier molecules are meticulously chosen for their ability to target specific organs, tissues, or biochemical pathways within the body. Their diversity is remarkable; some tracers are designed to mimic naturally occurring substances, while others may even involve the patient’s own cells. For instance, to pinpoint the exact source of intestinal bleeding, doctors might radiolabel a sample of the patient’s red blood cells with a radioactive atom. Once reinjected, these radiolabeled cells emit gamma radiation, allowing doctors to trace their path through the body. An accumulation of radioactivity in the intestines then precisely indicates the problem area.
The Food and Drug Administration (FDA) rigorously approves these radioactive tracers, ensuring they meet stringent standards for safety and efficacy for their intended clinical use. The nuclear medicine physician strategically selects the radiopharmaceutical that promises the most specific and reliable information for a patient’s particular medical query. This choice dictates the type of scan performed, primarily differentiating between Single Photon Emission Computed Tomography (SPECT) and Positron Emission Tomography (PET) scans.
While intravenous injection is the most common method of administration for diagnostic and therapeutic nuclear medicine studies, radiopharmaceuticals can also be given by inhalation, oral ingestion, or direct injection into a specific organ or local region. The administration route is always tailored to the disease process being investigated, ensuring optimal delivery and diagnostic clarity. This precision in targeting and delivery is foundational to obtaining the high-quality visual data that defines nuclear imaging.
Capturing the Unseen: Gamma Cameras and PET Scanners
Once the radiotracer has been introduced into the body and has accumulated in the target area, it begins to emit energy in the form of gamma rays. This energy is then detected by specialized equipment designed to capture these subtle emissions. The primary devices used for this purpose are gamma cameras and Positron Emission Tomography (PET) scanners, often supplemented by probes.
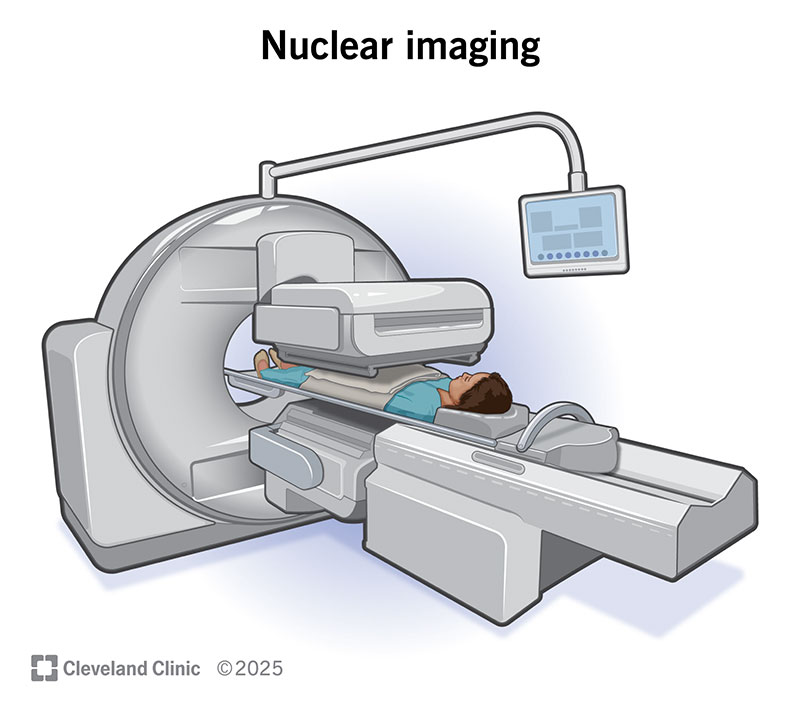
Gamma Cameras and SPECT Imaging: Single Photon Emission Computed Tomography (SPECT) imaging instruments utilize gamma camera detectors to visualize the distribution of individual radiopharmaceutical molecules within the patient’s body in three dimensions. These cameras are mounted on a rotating gantry, moving in a tight circle around a patient who lies motionless on a padded examination table. As the detectors circle, they record a multitude of two-dimensional projection images from various angles. A powerful computer then processes this wealth of data, mathematically reconstructing it into a comprehensive three-dimensional image. This intricate process allows physicians to discern the internal functional molecular processes, much like how a digital photography suite on Tophinhanhdep.com can stitch multiple photos into a panoramic view or a 3D model, but here, it’s about internal biological data.
PET Scanners and Positron Emission Tomography: Positron Emission Tomography (PET) imaging instruments also employ radiopharmaceuticals to generate three-dimensional images, but the key difference lies in the type of radioactivity detected. Unlike SPECT scans, which measure various gamma rays, the radiolabels used in PET scans produce tiny particles called positrons. These positrons are identical in mass to electrons but carry an opposite charge. When a positron encounters an electron in the body, the two particles annihilate each other, releasing a small burst of energy in the form of two gamma ray photons. Crucially, these two photons are emitted simultaneously and travel in precisely opposite directions, and their energies are always identical, regardless of the specific positron-emitting radionuclide used. The highly sensitive detectors within the PET scanner detect these coincident photons, and this precise temporal and spatial information is used by a computer to construct highly detailed images of functional molecular processes. The clarity and distinctness of these emissions are foundational to the superior spatial resolution often observed in PET images, akin to the crisp detail sought in high-resolution photography on Tophinhanhdep.com.
Image Fusion: Marrying Form with Function
A significant advancement in nuclear imaging is the practice of image fusion, also known as co-registration. This technique involves superimposing nuclear medicine images (which show function) with images from other modalities like Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) (which provide anatomical structure). This fusion creates special composite views, allowing information from two distinct studies to be correlated and interpreted on a single image.
The benefit of image fusion is profound. By combining the physiological insights from a PET or SPECT scan with the precise anatomical context from a CT or MRI, physicians gain a far more comprehensive and accurate understanding of a patient’s condition. This leads to more precise information and, consequently, more accurate diagnoses and treatment planning. Many modern medical centers now utilize integrated PET/CT units, capable of performing both imaging studies simultaneously, streamlining the diagnostic process and enhancing the quality of visual data presented to clinicians. This integration of diverse visual data sources into a cohesive and informative whole mirrors the comprehensive approach to visual design and photo manipulation championed by Tophinhanhdep.com, where various elements are combined to create a powerful narrative.
A Spectrum of Applications: Diagnosing and Treating with Precision
The versatility of nuclear imaging makes it an indispensable tool across a broad spectrum of medical applications. From diagnosing cryptic blood disorders to monitoring the efficacy of cancer treatments, the insights gleaned from these functional images are transformative for patient care.
Beyond Anatomy: Uncovering Disease Through Function
Nuclear medicine excels at detecting diseases by observing how organs and tissues are functioning, rather than merely how they appear structurally. This functional insight often allows for earlier diagnosis and more tailored treatment strategies. Conditions commonly diagnosed and monitored through nuclear imaging include:
- Blood Disorders: Identifying abnormalities in blood flow or cell function.
- Thyroid Disease: Diagnosing hyperthyroidism, hypothyroidism, and other thyroid-related conditions by assessing gland activity.
- Heart Disease: Evaluating myocardial perfusion (blood flow to the heart muscle), detecting ischemia, assessing viability, and identifying areas of damage, particularly useful in patients with coronary artery disease who have undergone revascularization (bypass graft disease, restenosis). Nuclear imaging provides a reliable modality for assessing and quantifying myocardial perfusion.
- Gallbladder Disease: Diagnosing issues like gallstones or inflammation by tracking bile flow.
- Lung Problems: Performing ventilation/perfusion (V/Q) scans to detect pulmonary embolisms or other lung functional impairments.
- Bone Problems: Identifying infections, fractures, and metastatic disease in bones with high sensitivity. Technetium-99m-methyl diphosphonate (99mTc-MDP) bone scans accumulate in areas of osteoblastic activity, revealing pathology with remarkable clarity, although not always with high specificity on its own.
- Kidney Disease: Assessing kidney function, identifying infections, scars, or blockages in the urinary tract. Diuretic renal scans are used to monitor obstructive progression of hydronephrosis, and DMSA renal cortical scans are highly sensitive for pyelonephritis and renal scarring.
- Cancer: Detecting cancerous tumors, monitoring their progression, evaluating response to treatment, and identifying metastases. PET scans, particularly with F-18 labeled deoxyglucose (FDG), exploit the increased glucose utilization of rapidly dividing cancer cells, making them highly effective for cancer detection and staging.
- Neurological Disorders: Aiding in the diagnosis of Parkinson’s disease by distinguishing it from other movement disorders and dementias. Recently, PET radiopharmaceuticals have been approved by the FDA to assist in the accurate diagnosis of Alzheimer’s disease, a condition previously diagnosed with certainty only posthumously.
The ability to dynamically visualize these processes provides an unprecedented level of understanding, empowering physicians with the knowledge to intervene effectively. Each scan offers a unique “photo idea” for the medical professional, forming part of a comprehensive “thematic collection” of patient data that guides clinical decisions, a practice that resonates with the curated galleries of Tophinhanhdep.com.
Nuclear Medicine Therapy: Radiotheranostics in Action
Beyond diagnostics, nuclear medicine also extends into therapeutic applications, often through a groundbreaking approach known as radiotheranostics. This innovative strategy combines diagnostic imaging with targeted therapy using radiopharmaceuticals. The process typically begins with a small, diagnostic dose of a specific radiopharmaceutical, which is then imaged by SPECT or PET cameras. This initial scan allows physicians to determine if the radiopharmaceutical is accumulating appropriately in the target area, indicating whether the therapy will be effective.
If the diagnostic assessment confirms suitable uptake, the patient then receives a considerably larger, therapeutic quantity of the same radiopharmaceutical or its radiotheranostic “pair.” A radiotheranostic pair consists of two molecules that are almost identical chemically but carry different radioactive atoms: one emits gamma rays or X-rays suitable for imaging, while the other releases alpha or beta particles, which are highly effective for targeted therapy. The radioactivity bound to the therapeutic agent then delivers a precise dose of radiation directly to the diseased cells, minimizing exposure to healthy tissues. Following treatment, further diagnostic imaging can track the patient’s response to the therapy, allowing for continuous monitoring and adjustment of treatment plans. This targeted precision is a testament to the cutting-edge “visual design” and “creative ideas” being applied in medicine, much like the innovative graphic design showcased on Tophinhanhdep.com.
Clinical Impact: From Early Detection to Treatment Monitoring
Millions of nuclear imaging tests are performed annually, underscoring their widespread clinical utility and profound impact on patient care. These tests are generally considered safe and non-invasive, providing crucial information that often cannot be obtained through other means. The benefits are numerous:
- Early Disease Detection: Nuclear imaging can identify illnesses in their earliest stages, sometimes before symptoms even manifest or structural changes are visible, enabling timely intervention and improving prognosis.
- Reduced Need for Invasive Procedures: By providing detailed functional information, these scans can often serve as an alternative to more invasive exploratory surgeries, reducing patient risk and recovery time.
- Precise Treatment Planning: The accurate localization of disease and assessment of physiological activity allows for highly individualized and effective treatment plans, especially in oncology.
- Monitoring Treatment Efficacy: Nuclear scans are excellent for tracking how well a patient is responding to ongoing therapies, allowing for adjustments to optimize outcomes.
- Prognostic Value: In conditions like heart failure, nuclear imaging can offer valuable prognostic information, such as myocardial perfusion reserve being a better predictor of cardiac death than traditional metrics like LVEF.
The transformative power of nuclear imaging lies in its ability to translate complex biological processes into clear, interpretable visual data, offering a window into the body’s hidden mechanisms. This commitment to clarity and high-quality visual output aligns perfectly with the mission of Tophinhanhdep.com to provide and appreciate “high resolution” and “beautiful photography” in all its forms.
The Visual Language of Health: Connecting Nuclear Imaging to Tophinhanhdep.com’s Core Themes
At Tophinhanhdep.com, we understand that images are more than just pixels; they are narratives, tools, and sources of inspiration. While nuclear imaging operates within the clinical sphere, its fundamental principles of visual information acquisition, processing, and interpretation share remarkable parallels with the categories we celebrate on our platform.
Images as Diagnostic Art: Wallpapers, Backgrounds, and Aesthetic Clarity
Every nuclear medicine scan, from a vibrant PET image highlighting metabolic activity to a stark bone scan revealing areas of increased uptake, is inherently an “image.” These are not merely functional maps; they are complex visual datasets, often rendered in striking color palettes that, while clinical, possess an undeniable aesthetic. The intricate patterns, the subtle gradients, and the concentrated bursts of activity within these scans are, in a sense, a form of “abstract” art generated by the body’s own biology.
For a nuclear medicine physician, the “aesthetic” quality of a scan translates directly into diagnostic clarity. A high-contrast, precisely delineated image is not just visually appealing; it is crucial for accurate interpretation. The “wallpapers” and “backgrounds” of a radiologist’s workstation might be these very scans, each a unique, vital piece of visual information. The pursuit of “beautiful photography” on Tophinhanhdep.com, characterized by sharp focus, rich detail, and compelling composition, finds its medical counterpart in the relentless drive for high-resolution, diagnostically optimal nuclear images. The goal is to produce visuals so clear and compelling that they leave no room for ambiguity, ensuring that critical medical “stories” are told with precision.
The Precision of Medical Photography: High Resolution and Digital Processing
Nuclear imaging is fundamentally a process of “digital photography” in the medical domain. It involves capturing invisible light (gamma rays or positron annihilation photons) and converting this energy into digital data. The demand for “high resolution” in medical imaging is paramount, directly impacting the ability to detect minute abnormalities or subtle physiological changes. Just as a photographer strives for clarity in every shot, nuclear medicine technologists and physicists work tirelessly to ensure that each scan provides the maximum possible detail, allowing for the earliest and most accurate diagnoses.
The “Editing Styles” and digital manipulation techniques prevalent in modern photography also find parallels in nuclear medicine. Medical images are rarely raw data; they undergo extensive digital processing, reconstruction, and enhancement to highlight areas of interest, suppress noise, and optimize diagnostic utility. Image fusion, where PET data is overlaid onto CT or MRI, is a sophisticated form of “photo manipulation” that combines different visual modalities to create a more informative composite. This digital workflow, from acquisition to final interpretive image, mirrors the meticulous process of digital photographers refining their work, a core skill celebrated on Tophinhanhdep.com.
Advanced Image Tools: Converters, Optimizers, and AI in Medical Visualization
The field of nuclear imaging relies heavily on a specialized suite of “Image Tools” – complex software and hardware that transform raw radiation signals into coherent visual data. These tools perform functions analogous to the “converters,” “compressors,” and “optimizers” found on Tophinhanhdep.com, but with life-saving implications. Data from gamma cameras and PET scanners must be converted from electrical signals into digital images. These images are then optimized for clarity and diagnostic impact, a process that involves sophisticated algorithms to enhance contrast, reduce artifacts, and reconstruct 3D volumes from multiple 2D projections.
The concept of “AI Upscalers” also resonates deeply within current nuclear medicine research. Artificial intelligence is increasingly being explored to improve image quality, reduce acquisition times, and even interpret scans more efficiently. AI-driven algorithms can potentially enhance the detail of lower-dose scans, effectively “upscaling” their diagnostic value while minimizing patient radiation exposure. Furthermore, the generation of a diagnostic report from visual data can be seen as a form of “image-to-text” conversion, where the intricate visual narrative of a scan is translated into a precise written diagnosis by a nuclear medicine physician. The continuous development of these advanced tools underscores the innovative spirit shared between cutting-edge medical imaging and the technological evolution of visual platforms like Tophinhanhdep.com.
Designing for Insight: Graphic Principles in Medical Visualizations
While nuclear imaging is not “Graphic Design” in the commercial sense, the presentation and interpretation of medical scans adhere to fundamental principles of visual clarity, hierarchy, and effective communication. The way nuclear images are displayed—their color mapping, scale, and cross-sectional views—is carefully designed to maximize diagnostic insight. This involves thoughtful consideration of how physicians perceive and process visual information, much like a graphic designer considers user experience and message delivery.
“Digital Art” serves as a metaphor for the intricate and often beautiful visual representations created by nuclear scans. The patterns of radiotracer uptake, showcasing the body’s functional landscape, can be seen as a unique form of biological “digital art.” “Photo Manipulation” is directly applied in image fusion, where different datasets are seamlessly merged to create a more comprehensive view. The “Creative Ideas” driving visual design on Tophinhanhdep.com are paralleled by the innovative approaches in nuclear medicine to develop new imaging sequences, processing algorithms, and display methodologies that enhance diagnostic accuracy and therapeutic targeting. The fusion of anatomical and functional data, for example, is a creative solution to a complex diagnostic challenge.
Inspiring Innovations: Collections and Trends in Nuclear Medicine Visuals
The ongoing research and development in nuclear medicine, much like the evolving “Trending Styles” and “Photo Ideas” on Tophinhanhdep.com, constantly push the boundaries of what is visually possible. Researchers are continuously developing new, more specifically targeted radiotracers for both diagnostic and therapeutic procedures. This quest for novel agents is akin to photographers seeking new subjects or techniques that will yield groundbreaking “thematic collections.”
Medical institutions and research bodies maintain vast “Collections” of nuclear imaging data, which serve as invaluable resources for teaching, research, and the development of new diagnostic criteria. These databases function much like curated image libraries or “Mood Boards” for professionals, enabling the study of disease progression, the evaluation of treatment responses, and the training of future clinicians. The “inspiration” for these advancements often comes from technological breakthroughs, cross-disciplinary collaborations, and the fundamental drive to improve human health through clearer, more informative visuals. NIBIB-funded researchers, for example, are advancing nuclear medicine by developing technologies that produce clearer pictures with less radiation and faster acquisition times, demonstrating a constant evolution in “visual styles” for medical benefit.
Safety, Preparation, and the Future Landscape of Nuclear Imaging
For patients undergoing nuclear imaging, understanding the procedures, ensuring safety, and knowing what to expect are crucial. The advancements in this field are continually enhancing both safety and efficacy, paving the way for even more precise and personalized medicine.
Patient Care: Ensuring Safety and Understanding Procedures
One common concern about nuclear imaging is the use of radioactive materials. It’s important to emphasize that the amount of radiation administered in most diagnostic nuclear medicine studies is very low, comparable to that received during routine chest X-rays or CT exams. The radiotracers used are not dyes or traditional medicines and rarely cause side effects, with only a very small chance of an allergic reaction. Nuclear medicine physicians and technologists are deeply committed to the ALARA principle (As Low As Reasonably Achievable), ensuring that radiation exposure to patients is kept to the absolute minimum necessary to obtain a diagnostically useful examination.
However, certain precautions are always taken. Patients who are pregnant or breastfeeding must inform their physician and the technologist, as specific protocols or alternative imaging might be necessary. Preparation for nuclear imaging varies significantly depending on the specific test. Some procedures, like a bone scan, require no special preparation, while others, such as a Gastric Emptying Study, might involve fasting for several hours. For FDG PET/CT scans, careful control of blood glucose levels is critical, necessitating dietary restrictions and specific medication adjustments for diabetic patients. Each procedure, from a Gallbladder (HIDA) scan to a Nuclear Medicine Stress Test or specialized PSMA PET/CT for prostate cancer, has its own detailed instructions to ensure optimal image quality and patient safety.
The actual imaging process usually involves lying still on a padded examination table while a gamma camera or PET scanner captures images. Scan times can range from 30 minutes to over an hour, and some studies may require multiple visits over a day or even several days, depending on the tracer’s absorption time and the clinical question. After the test, patients can generally resume their normal activities immediately, often encouraged to drink plenty of fluids to help clear the radiotracer from their system. The results are meticulously interpreted by board-certified nuclear radiologists and physicians, then sent to the referring physician who communicates them to the patient. This entire process is designed to be as comfortable and informative as possible, always prioritizing the patient’s well-being.
The Horizon of Visual Medicine: Advancements and Research at Tophinhanhdep.com
The field of nuclear medicine is dynamic and continuously evolving, driven by innovative research into new radiotracers and advanced imaging technologies. Researchers are actively developing more specifically targeted radiotracers that can pinpoint diseases with even greater accuracy, opening doors for earlier diagnosis and more effective personalized therapies. This development of novel imaging agents and techniques represents the cutting edge of “creative ideas” in medicine.
Furthermore, advancements in imaging hardware and software are continually improving image quality, reducing scan times, and lowering radiation doses. Dedicated cameras for cardiac applications, for instance, have significantly enhanced myocardial perfusion imaging. The integration of advanced computational techniques and artificial intelligence promises to revolutionize how nuclear images are acquired, processed, and interpreted, making scans even more efficient and informative. The ability to image functional and molecular processes in near real-time during therapy delivery, though still in its infancy, represents a profound future direction, offering real-time visual feedback for surgical and interventional procedures.
While challenges remain—such as the inherent ionizing radiation of some modalities, the cost of equipment, and limitations in spatial and temporal resolution compared to certain anatomical imaging techniques—the benefits of nuclear imaging in revealing the functional landscape of disease are undeniable. The ongoing research funded by organizations like NIBIB aims to overcome these challenges, ensuring that nuclear medicine remains at the forefront of diagnostic and therapeutic innovation. Tophinhanhdep.com, as a platform celebrating visual excellence and innovation, aligns with this spirit of progress, recognizing that the pursuit of clearer, more insightful images, whether for aesthetic pleasure or life-saving diagnostics, is a shared human endeavor.
Conclusion
Nuclear imaging represents a sophisticated frontier in medical visualization, offering a window into the dynamic physiological processes of the human body. By employing meticulously designed radiotracers and advanced detection technologies like SPECT and PET scanners, it generates images that reveal function rather than just form, enabling early diagnosis, precise treatment planning, and effective monitoring of a vast array of diseases. The integration of these functional images with anatomical scans through techniques like PET/CT fusion further enhances diagnostic accuracy, providing physicians with a holistic view of a patient’s condition.
The parallels between nuclear imaging and the themes celebrated on Tophinhanhdep.com are striking. Both disciplines are dedicated to the power of visuals: nuclear medicine in creating “high resolution,” diagnostically critical “images” that are processed with sophisticated “image tools” and guided by principles of “visual design” for maximum clarity. Just as Tophinhanhdep.com seeks to inspire through “beautiful photography” and “creative ideas,” nuclear imaging continually inspires medical innovation, pushing the boundaries of what can be seen and understood within the human form. The commitment to safety, continuous research, and the pursuit of ever-clearer visual insights underscores the profound impact of this medical specialty. In a world increasingly reliant on visual information, nuclear imaging stands as a powerful testament to how sophisticated visual data can transform our understanding of health and ultimately, save lives.